Sunday, October 28, 2007
Still Ticking
My stamina and physical endurance are better that than they were pre-EECP therapy. I sleep better at night and have not taken naps in the day. My mobility is better. I get out of bed with much less struggling than before and most of problems I do have moving I attribute to my Parkinson's disease.
I would recommend EECP to anyone who has coronary artery disease and who do not want to undergo the traumatic and invasive surgical coronary artery bypass graft. Three years and seven months ago, I was told by a cardiologist that I was a walking time bomb. He wanted me to undergo a quintuple bypass two days later. I decided to get a second opinion and am certainly glad I did.
If anyone wants to ask questions about my EECP experience or any other aspect of my experience with angina and coronary artery disease, please leave a comment.
Tuesday, October 02, 2007
The Countdown Begins

Well, just ten more therapy sessions and I'll be done with my EECP. While the results are not yet what I had hoped them to be, the angina has decreased in frequency, length and intensity. I haven't used nitroglycerin in at least a week. My stamina is generally better although I do take a short nap most days and I didn't before beginning EECP.
I had hoped I might have a complete absence of angina symptoms as I did for over two years on Dr. Wayne's medication regimen. I would definitely say so far EECP has been a success so far.
Friday, September 21, 2007
A Junkie's Brain & Parkinson's
From Wired.com
ATASCADERO, California -- In Monterey County Jail, in the spring of 1981, a 21-year-old drug dealer and junkie named Toby Govea lay in bed shaking violently and uncontrollably. Thanks to a bad batch of homemade heroin, Govea had developed symptoms of Parkinson's Disease, an incurable neurological illness that causes muscle rigidity, tremors and eventually loss of movement.
Today, Govea remains incarcerated -- but free of tremors, thanks to a treatment made possible by research on the prisoner's own brain.
The treatment, called deep brain stimulation, has become the leading surgical treatment for Parkinson's, which afflicts 1.5 million Americans. It has been performed on more than 20,000 patients in the past decade.
In July of this year at the Atascadero State Hospital in California, Govea was lucid, and his muscles were still, as he recalled the events that made him a human guinea pig who helped develop a treatment for his own illness.
As I create this post, I am leaving the errrors that my Parkinson's diease creates through my tremors. This is tod emonstrtae how debilitating the condition can be, espcially to one who writes for a liviingg or as an avocation. Articles I submit fofr publicattion have too be meticuloussly edited before submissioon.
There was a time when my L-Dopa/Carbidopa controlled my symptoms for six hours at a time. Since I took it four times a day, that meant an absence of tremors for 24 hours a day. Now themedicaation works about four hours at a time, leaving me with two hours of significant symptoms -- severe leg a nd arm tremors, difficulty swallowing and ambulating, legs freezing when I walk, especially turing corners and arms freezing when I try to hang clothes in the closet.
Right now I am undegoing EECP for my coronary artery disease. I fear this therapy, which h as signficantly lessened my angina symptoms may be contributingn too my Parkinson's symptoms. I guess I won't know until the therapy is completed next month and I check in with my neurologist back in Indiana. I will keep you posted.
Monday, September 10, 2007
10th EECP Session
When my cardiologist, Dr. Ken LeClerc, examined me before I started EECP, he told me after the 35 consecutive hour-long sessions, he may be able to take me off of some of the medication. I asked if that might mean I could stop taking my beta-blocker and could begin using Viagra or Cialis again. He told me I may not need those drugs to maintain an erection after EECP.
Now as I said above, this feeling may be psychological on my part, but since starting EECP, I have gotten an erection during almost each therapy session. I also am happy to report I have been able to function more than adequately the few times I have engaged in intercourse since beginning EECP.
This therapy, in my opinion, is a logical substitute for coronary artery bypass surgery. It is far less expensive and dangerous as the surgical alternative, not to mention less traumatic to the body. EECP has virtually no contraindications and the side effects are limited to some chafing of the skin, which I have yet to experience.
Anyone who takes the time to read this entire blog from beginning to end will realize I have taken a careful and studied approach to treating my own coronary artery disease and angina. I refused to allow an invasive cardiologist, whom I consider a medical terrorist, to coerce me into getting a quintuple bypass. The medical approach prescribed by Dr. Howard Wayne gave me three years without having to recover from surgery.
Now I have chosen EECP to treat my returned angina symptoms. This therapy, much like Wayne's medical approach, assists the body in creating natural bypasses around clogged arteries. I should enjoy another four to five angina-free years and EECP is a noninvasive treatment that can be performed in a year if necessary. The surgery that the medical terrorists tried to coerce me into in my 56th year, may not need to be done until I am 65 or 69 if lucky.
If you have a greedy cardiologist trying to scare you or your loved ones into bypass surgery, please seek out a second opinion from a noninvasive cardiologist. What do you have to lose?
Thursday, August 30, 2007
EECP & Me
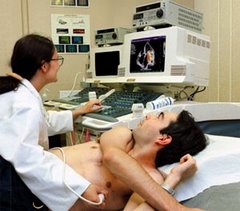
Velcro-secured wraps are placed securely around the legs and lower torso. They squeeze your body every time the heart is at rest. Yesterday Daphne took the pressure up to 6 psi, the maximum therapeutic level.
All of the literature says not to expect to feel any positive results until you have completed around a dozen of the 35 sessions. Well, it may be my imagination, but my tolerance for exercise seems much better and I have had to use nitroglycerin twice since Monday.
It has been a long arduous road from the time I decided to take charge of my own body in 2004. In April of that year, an Indianapolis cardiologist characterized me as a walking time bomb (see the beginning of this blog for more information) unless I had a quintuple coronary artery bypass. I got a second opinion and the rest is history.
To recap, it has been more than three years since I declined to receive the bypass. The EECP will give me another 4 to 5 surgery-free years. That means my life will maintain some semblance of untraumatic normalcy for a total of 8 to 9 years.
American doctors, especially invasive cardiologists and their cardio-thoracic surgeon allies are too quick to cut. Their decisions re based more on the personal finances of the physician and the greed of the hospital they work in.
I agree with the late Dr. Howard Wayne's label of these doctors as "Medical Terrorists." I sincerely believe they use their license to practice medicine as a license to commit assault with a deadly weapon. What else would you call unnecessary invasive surgery you are coerced into receiving?
Thursday, August 16, 2007
Orientation
The first thing I did was watch a video that gave me an overview of what EECP is, how it is performed, expected results, etc. It wasn't anything i hadn't already studied about, but the presentation, produced by the manufacturer of the equipment used in doing EECP, was professionally done and accurate.
Next, we filled out some questionaires regarding symptoms and Daphne fitted me for a pair of tights which are worn when receiving EECP. I will return to the clinic on Monday 20 August for my first session. Patients usually don't feel any results the first ten or so sessions, but I will report how mine went whenever there is something interesting happening.
Wednesday, August 08, 2007
My EECP Begins Soon
I arrived in the Alamo City last Friday to continue the search for someone who will prescribe a course of EECP. I started in Indianapolis where the cardiologists who would prescribe it also required an angiogram. Anyone who has read my site knows what I think of angiograms.
The only tests Dr. LeClerc required were vital signs and an EKG. He does want copies of all the lab work my primary care physician in Indianapolis has in my records.
I should begin my EECP on Monday, 13 August. It takes 35 sessions over seven weeks to finish the therapy, but there is an at least 85% chance it will be successful and my angina symptoms will be controlled for at least five years.
It was a little more than three years ago I started on the late Dr. Howard Wayne's medical regimen. If indeed EECP gives me five more years, I will have lived eight years longer than the cardiologist who wanted to subject me to a quintuple bypass in 2004 said I would.
Sunday, July 29, 2007
Letter
Hello Jeff,
I was reading your blog today. I´m sorry to know that Dr. De Vries is leaving his practice.
And I´m sorry that every doctor wants to do an invasive test in order to prescribe EECP to you.
We are also still seeking a real noninvasive Cardiologist, we haven´t find one yet. Every potential doctor does not want to hear about anything but CABG for my husband.
All this is almost unbelievable :-( , but sadly very true not only in the USA, but at least in Mexico too.
Have you talked to Gypsy? We talked to her last February. she said she was actively trying to find someone interested to buy Dr Wayne's practice. We haven´t heard from her since then.
I´m constantly searching information in the Internet, I ´ve found a few doctors that call themselves noninvasive.
I have not talked to any of them, so I don´t know how true is that. I want to share their names with you, probably you already know them. Maybe one of them can help you.
I was thinking that probably this Dr. Chung could prescribe you the EECP treatment. I don´t know anything else about him than what he has posted in that Cardiology forum, but at least he says he would respect the patient decisions.
There is also this noninvasive center that prescribes EECP: http://whitakerwellness.com
Another noninvasive Cardiologists: Dr. Thiak: http://www.drthaik.com/ , Dr. Gould : http://www.uth.tmc.edu/pet/ , Dr. William R. Davis http://heartscanblog.blogspot
My best wishes in your search.
Best regards from Mexico City.
Maria
EDTA vs EECP
| Originally Posted by Cannuck Chelation has been used for many decades for a variety of reasons. My wife's Aunt was treated with EDTA for the aftereffects of the concentration camps, as were German citizens from the Ruhr Valley for heavy metal poisoning. I personally know seniors who have done so here for various cardiovascular conditions (most with significant success), and can tell you that the results are VERY short in coming. |
When I said EDTA (Chelation therapy) either oral or IV is controversial, that doesn't mean I disapprove of it. Quite the contrary, I feel it is a choice of treatments that has been effective in treating CAD and some other coronary diseases and despite the fact it hasn't been approved by the FDA for use in such diseases, should be available to patients making informed choices. The reason I am opting for EECP is because I have studied its effects, side effects and contraindications and have talked with patients who have received it. Unlike bypass surgery "victims" and angioplasty (balloon & stent) recipients, none of them had negative reports of their experiences.
Further, angiogenesis and the development of a collateral vessel system to naturally bypass the clogged coronary arteries is a process the body already has started on its own, without the introduction of any drug. Like it or not EDTA is a drug and therefore could have side effects or be harmful. There are reports of unexpected deaths during or following chelation therapy. I have found none associated with EECP. That is not to say EECP recipients haven't died as a result of therapy, there simply are no reports where the therapy caused the deaths, that I have found.
I realize EDTA is a natural enzyme and as such can be sold as a nutritional supplement and I am not opposed to nutritional supplements as long as they are used wisely and in some form of a therapeutic regimen. I personally take the following supplements daily in the strengths and doses indicated:
Organic Flaxseed Oil 1200 mg, three times a day
Borago Seed Oil 1200 mg, three times a day
Omega 3 Fish Oil 1200 mg, three times a day
d-Alpha Tocopheryl (Vitamin E) 400 IU, one time a day
Glucosamine 750 mg Chondroitin 600 mg, twice a day
Folic Acid 800 mcg, one time a day
B-100 Ultra B-Complex, one time a day (Puritan's Pride Brand)
l-Arginine 500mg, one time a day
Super C Complex 1000 mg, three times a day (Puritan's Pride Brand)
Acetyl L-Carnitine 400 mg with Alpha Lipoic Acid 200 mg, one time a day
Natural Selenium 50 mcg, four times a day
Co-Enzyme Q10 100 mg, one time a day
Magnesium Oxide 400 mg, one time daily
Multiple Vitamin, one time daily
I always try to take my supplements with food and I am on a schedule that has me taking something, prescribed medications and supplements every six hours.
Just for the information to folks with CAD and angina, my medical treatment regimen is aimed at not only controlling my blood pressure, but keeping it as low as possible without adverse side effects. I try to keep mine around 90/50 when I am at rest. It usually ranges between 80/40 to 100/50. When my BP is a normal 120/70 or more, during stress or increased physical activity, I often experience symptoms of angina. Here are the prescribed drugs I am on daily
Aspirin 325 mg in the morning
Fosinopril
Metopropolol Tartrate
Isosorbide Mn
Nitroglycerine (as needed)
No dosages are provided because you need to consult a physician before starting this protocol. Suffice it to say, some of the dosages are higher than usually recommended. The Isosorbide and Nitroglycerine were recently added to my regimen and Modiuretic was discontinued due to an abnormal increase in blood tests that indicated my liver was being adversely affected. I also take prescription medication for Parkinson's disease.
I cannot emphasize enough the need to be under the care of a medical doctor who you trust and have a good working relationship with. I encourage anyone who has CAD or angina or has a loved one who does to read my blog from beginning to end and to get a second opinion from a non-invasive cardiologist before being coerced into bypass surgery they do not need.
Saturday, July 28, 2007
One More Opinion About EECP

A noninvasive procedure for treating angina has proven nearly as effective as angioplasty, said a cardiologist who has been using Enhanced External Counterpulsation for his patients for the past several years.
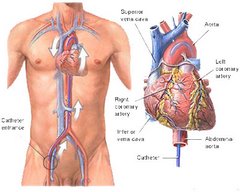
Dr. James P. O’Neil, a cardiologist with the Cardiology Group, which administers the procedure at its Mount Laurel office, said coronary angioplasty, a medical procedure which involves inserting a balloon catheter to open a blockage in an artery, and the EECP offer patients “about the same success rate.”
During EECP, cuffs similar to blood pressure cuffs that have been wrapped around patients’ legs are inflated and deflated, forcing blood to flow through arteries. “The body reacts by improving collateral blood flow” with small capillaries expanding to compensate for the blocked artery, said O’Neil.
He said the aim of both procedures is to “improve exercise tolerance and fatigue,” common problems for heart patients.
Angina is a symptom related to coronary heart disease. Blockages in coronary arteries created by the buildup of plaque on the inner walls of the vessels limit the supply of oxygen-rich blood to the heart and cause the chest pain or discomfort known as angina and shortness of breath.
O’Neil said medications are usually the first step in an attempt to ease the discomfort, but if they do not work, then cardiac bypass surgery, angioplasty or EECP treatments should be considered.
He said EECP relieves symptoms in 75 percent of cases, “a little bit less than angioplasty,” which eases symptoms in 80 percent of cases. Cardiac bypass surgery improves symptoms 90 percent of the time, said O’Neil.
O’Neil said The Cardiology Group, which has five offices in Burlington County, has done nearly 300 of the lower risk EECP procedures since it began offering EECP six years ago. The procedure is administered the same now as when it was introduced, in one-hour sessions five days a week for seven weeks.
The time commitment is the only disadvantage of using EECP, said O’Neil, who cited several advantages of using it instead of angioplasty to relieve angina.
“Angioplasty is three times the cost as the EECP, the risk is higher, there is no survival advantage of angioplasty over EECP,” said O’Neil.
O’Neil said a report issued during a recent American College of Cardiology conference supported the view that the two procedures offer similar success.
“We used to think that people lived longer (by having angioplasty),” he said. “Angioplasty is really stretching the vessel and really tearing the vessel. During angioplasty, that vessel is damaged and as it heals, it can cause a scar.”
The resulting scar can create a new blockage, although a drug-eluding stent sometimes is used to hinder the scar buildup, he said.
“One out of 10 patients tend to block up again with that artery,” he said. “With EECP, we’re not damaging an artery and causing scar tissue to build up.
“The big thing that has been found with EECP, a patient is not going to die any more often than those who have angioplasty. There’s a big misconception that if we do angioplasty it’s going to make them live longer.”
An exception, he said, is that when performed during a heart attack, angioplasty can serve as a lifesaving procedure.
O’Neil compared the effectiveness of the three procedures used in relieving angina. He said cardiac bypass surgery improves symptoms in 90 percent of cases, angioplasty in 80 percent and EECP in 75 percent.
The cardiologist said some insurance carriers, including Medicare, only recommend EECP as a remedy for patients who are not considered candidates for cardiac bypass surgery or angioplasty.
“I and many physicians don’t agree. We think EECP should be offered along with bypass and angioplasty,” O’Neil said. “One of the reasons patients don’t want bypass is they are afraid.”
He said insurance regulations sometimes deter patients from taking advantage of EECP.
“One of the biggest obstacles is how the insurance companies can make it difficult. They can and do make it difficult for patients to go through this,” said O’Neil, noting that out-of-pocket charges such as per-visit co-pays can deter patients from having the treatments.
“They might not have as big an out-of-pocket expense if they take the riskier, higher priced procedure,” he said.
O’Neil said EECP costs $6,000 to $7,000 whereas the angioplasty costs $20,000 to $30,000.
Patients who have had EECP say they are happy with the results.
That includes the Cardiology Group’s first EECP patient.
At 83, Nick Russo still mans a tractor to cultivate the pumpkin patch at the family farm in Chesterfield. In March 2001, he was the first patient to undergo EECP at the Cardiology Group.
Although Russo stashes a bottle of nitroglycerin pills in his pocket — just in case — the Westampton man said he hasn’t needed any of the medication since 2003, when a second round of EECP treatments seemed to ease the lingering angina.
Russo, who was diagnosed with a heart problem 10 years ago, underwent an open heart procedure at Deborah Heart and Lung Center in Browns Mills, Pemberton Township, in 1999. He took nitroglycerin to ease angina, eventually deciding to have the EECP.
Russo said his initial EECP treatments were “a little frightening at first. You get a shock.”
After having the EECP in 2001, Russo said, “I would still get out of breath. Once in awhile I would have to take a nitro pill.”
He said he noticed the angina “when I would do anything that was exertion” — lifting bags of fertilizer, loading crates of corn — and his cardiologist suggested a second set of treatments.
Marlene Donnelly of the Cardiology Group said EECP can be repeated “as long as it’s medically indicated.” She said one patient has had three sessions of EECP.
Angioplasty also may be repeated, Donnelly said.
After having a second angioplasty last July (the first was in May 2006), Edward Stickel of Delanco “felt better for a while, and then I started to experience unstable angina. For about 11 consecutive days in September and October I had angina in my left shoulder,” he said.
Stickel, 68, said cardiologist Samuel Ventrella thought EECP would help. He started the treatments on Nov. 6, and after about 12 sessions “started to feel much better.” By Dec. 6, “I stopped having the angina,” said Stickel, who retired from teaching at Palmyra High School, where he also coached freshman football for 18 years. He enrolled in the Cardiology Group’s rehab program, and exercises at the Mount Laurel center twice a week.
The former educator also said he is still able to go waterfowl hunting and fly fishing.
Stickel said he is covered by Medicare and by a Blue Cross/Blue Shield plan and was not troubled by the cost of the EECP treatments.
“I was charged a $5 co-pay, which I found to be not a real problem,” he said.
Jane Tabone-Yerkes of Pemberton Township, who is covered by a Civil Service insurance plan, said she had no co-pay for her EECP treatments, which she completed on Feb. 5.
Diagnosed with a heart problem 17 years ago, Tabone-Yerkes, 76, said, “I feel wonderful. I can go up the steps, I go up and down and I have no problem.”
Tabone-Yerkes, who had a stent inserted following a heart attack in 2005, said she asked her cardiologist for the EECP after reading about the procedure in a magazine. She said a second bypass surgery was not recommended.
During the procedure, “You are plummeted,” said Tabone-Yerkes, describing the sensation.
“It’s like a boxer socking you in every blood vessel of your body, but it was not hard to take,” she said.
Tabone-Yerkes said her angina, which she felt “down one arm,” “disappeared completely after 15 sessions.
“I felt like I did when I had the bypass 17 years ago,” she said.
A nitroglycerin tablet is part of her daily pill regimen, which also includes medications to control diabetes, high cholesterol and high blood pressure. Tabone-Yerkes, who retired from her job as an accounting technician at McGuire Air Force Base, said a low-fat diet and swimming five laps each morning in her pool helps her stay fit, and she recently joined a fitness center that caters to cardiac patients.
She said EECP was a good choice.
“They used to say it’s the last resort, but I don’t think that’s true,” said Tabone-Yerkes.
(from the Burlington County Times)
Don't Believe Your Cardiologist
Big Dave
No matter how you do it, removing the plaque buildup is the cure to most coronary disease. A pharmacological cure would put a lot of heart surgeons out of business.
Actually that's not so, especially for males over 50. We have an uncanny ability to grow collateral vessels through a process called angiogenesis. Now if you have cancer, angiogenesis is a bad thing. It is responsible for the cancer traveling, becoming malignant. In those of us with coronary artery disease, the process actually helps the growth of collateral vessels. That is why, for the great majority of patients with coronary artery disease, a bypass does more harm than good because it destroys our natural bypass.
Regarding the pharmacological cure: if a cardiologist tries to coerce you into a bypass immediately after you have been diagnosed with CAD, believe me, he doesn't have your best interests in mind. Your interests are far behind the interests of the cardiologist, cardio-thoracic surgeon and his team, the hospital, the therapists, etc. A CABG is the most commonly performed and lucrative cardiac surgical procedure. The American Heart Association and the American College of Cardiologists have both officially stated a CABG should be a last resort, after medication and lifestyle change. Yet, most of these medical terrorists whho try to scare, and usually succeed, into scaring you and your wife into having your chest split open, will use every trick in the book to make you think a heart attack, stroke or death are imminent if you don't have an immediate CABG. That is a bald face lie.
I have challenged these blood sucking scum to debate me on my website or any forum of their choice. They do not even acknowledge the challenge because they know such an event would expose them for the charlatans they are.
That challenge still stands. I am not a physician. I am not even a current medical professional, though I was a nurse in the Army for 20 years and have worked for more than 15 years as a safety officer and senior medic on oil rigs. How about it, you medical terrorists who scare your patients into making your Mercedes and pool payments, care for a debate?
Your EECP Questions Answered
What is Enhanced External Counter-Pulsation (EECP)?
The Cleveland Clinic defines EECP as a treatment for those with symptomatic coronary artery disease, not eligible for standard treatments of revascularization. During EECP, cuffs wrapped around the calves, thighs and buttocks are inflated and deflated, gently but firmly compressing the blood vessels in the lower limbs, increasing blood flow to the heart. EECP may stimulate the openings or formation of collateral vessels to create a “natural bypass” around narrowed or blocked arteries.
The Sanger Clinic further defines EECP as a non-invasive procedure for patients with severe refractory angina… (It) can relieve or eliminate angina in patients who are not candidates for angioplasty or bypass surgery.
How does EECP work?
That’s a good question. EECP is designed to relieve angina by improving perfusion in areas of the heart deprived of an adequate blood supply. The cuffs inflate during diastole, the period when the heart muscle relaxes and the chambers fill with blood. The cuffs inflate sequentially from the calves upwards, resulting in increased pressure in the aorta and coronary arteries. Compression of the vascular bed in the legs also increases the return of venous blood to the heart and increases cardiac output. Patients are customarily treated with EECP for an hour a day for a total of 35 hours.
What is the history of the use of EECP in the USA?
The concept of counterpulsation is not new (it was first introduced in the late 1950s at Harvard), but the computerized technology currently available with EECP makes it a relatively new procedure, introduced less than 10 years ago. As of 2003 it is available in only about 200 centers across the United States.
EECP is used to treat patients with chronic stable angina, coronary artery disease, or high blood pressure. Most recently, the Food and Drug Administration (FDA) has approved EECP for the treatment of congestive heart failure. The treatment may be appropriate for patients who are not eligible for such non-surgical interventional procedures as balloon angioplasty, stent placement, rotoblation, atherectomy, or brachytherapy. It may also be used for patients who do not qualify for such surgical treatment as coronary artery bypass graft surgery.
EECP is not the first-line treatment for angina. Rather, it is reserved for patients who have not achieved good results from medication or interventional management of their symptoms.
EECP may benefit patients with such other medical conditions as erectile dysfunction, kidney disease, eye disease, diabetic neuropathy, and other circulatory disorders. More research is needed to evaluate the outcomes of EECP for these patients.
Are there any contraindications for EECP?
EECP is not recommended for patients who have certain types of valve disease; uncontrolled arrhythmias (irregular heart rhythms); severe hypertension; uncontrolled congestive heart failure; significant blockages or blood clots in the leg arteries; or those who have had a recent cardiac catheterization, angioplasty, or bypass surgery.
Are there any risks or side effects?
EECP is a relatively safe and effective treatment, and few adverse side effects have been reported. The main adverse side effect is chafing (skin irritation from the compression of the cuffs). To reduce or prevent this side effect, patients are instructed to wear tight-fitting cycling pants or athletic tights. Leg pain is another adverse side effect.
What are the normal results?
The benefits of EECP are comparable to the results of angioplasty and coronary artery bypass graft surgery: 80% of patients experience significant improvement after EECP treatment. The largest research study on EECP indicates that after receiving treatment, patients used less medication, had fewer angina attacks with less severe symptoms, and increased their capacity to exercise without experiencing symptoms. EECP improves the patient's sense of well-being and overall quality of life; and in some cases, prolongs the patient's life. Benefits five years after EECP treatment are comparable to surgical outcomes.
The effects of EECP treatment last from three to five years and sometimes longer.
EECP does not prevent coronary artery disease from recurring; therefore, lifestyle changes are strongly recommended and medications are prescribed to reduce the risk of recurrent disease.
What sort of lifestyle changes are we talking about?
These are changes you already have, or should have taken:
- Quitting smoking. Smoking causes damage to blood vessels, increases the patient's blood pressure and heart rate, and decreases the amount of oxygen available in the blood.
- Managing weight. Maintaining a healthy weight, by watching portion sizes and exercising, is important. Being overweight increases the work of the heart.
- Participating in an exercise program. The cardiac rehabilitation exercise program is usually tailored for the patient, who will be supervised by professionals.
- Making dietary changes. Patients should eat a lot of fruits, vegetables, grains, and non-fat or low-fat dairy products, and reduce fats to less than 30% of all calories. Alcoholic beverages should be limited or avoided.
- Taking medications as prescribed. Aspirin and other heart medications may be prescribed, and the patient may need to take these medications for life.
- Following up with health care providers. The patient needs to visit the physician regularly to control risk factors.
Sunday, July 22, 2007
A Letter to the Editor about EECP
Dear (Napa Valley Register ) editor,
This is a belated thanks to Dr. Dizman, Napa cardiologist, and nurse Susan Hart for giving me medical service that changed my life and avoided the problems that come with bypass surgery.
For some time before October 2001, I was suffering periodic chest pains. I finally went to a cardiologist (not Dr. Dizman) who after an examination scheduled me for a bypass operation. Before I had the operation, I went to see Dr. Dizman about his non-invasive heart treatment program, Enhanced External Counter Pulsation.
I canceled by scheduled bypass operation and started the EECP therapy given by nurse Susan Hart. After completing the 35 daily sessions, my chest pains were gone, and I haven’t had any problems since then. I strongly recommend that anyone thinking about getting a bypass operation check out the EECP therapy available at Dr. Dizman’s medical center. If it doesn’t help, you can always get a bypass operation. Medicare paid for the EECP therapy, so it must be an approved medical program.
John J. Eberle / Napa
Seeking a Noninvasive Cardiologist
If you have not read my blog from the beginning, you may not understand why I am so adamant about this. Let me briefly bring you up to date and encourage you to read my entire blog.
In April 2004, I was diagnosed with coronary artery disease (CAD) which I was told was the cause of the angina I had been experiencing for about six months. The interventionalist cardiologist my family doctor sent me to, tried to coerce me into an immediate quintuple CABG, despite the fact, that as he put it, my heart was "in great shape." He wouldn't tell me how my heart could bee in great shape when the arteries that were providing it oxygen were 85 to 100 percent blocked.
He did try to schedule me for the quintuple CABG on Thursday, two days later. When I told him I wanted a second opinion, he told me I was a "walking time bomb," and that I could "have a heart attack, stroke, or even die within three months." I replied that I had been experiencing angina for six months and would take the risk.
I'm glad I did. I sought out the opinion of Dr. Howard Wayne of the Noninvasive Heart Clinic in San Diego. To make long story short, he evaluated me and started me on medical treatment I remain on until this day, three years and four months later.
Unfortunately, in November 2006, the angina returned while I was running to make a connection at Charles De Gaulle Airport in Paris. I contacted Dr. Wayne's clinic and sadly learned he had passed away three weeks earlier. (Lest anyone assume he was the victim of heart disease, Dr. Wayne died while climbing mountains near Lake Tahoe. He was 83.)
I saw a doctor in Chicago who agreed to follow the protocol set up by Dr. Wayne, although he did feel I should have the CABG. He also thought I might benefit from Enhanced External Counterpulsation. EECP is a noninvasive therapy.
My doctor in Chicago is leaving his practice and I can not find a cardiologist in Indianapolis that will prescribe EECP unless I undergo an angiogram. Readers of this blog will understand why that is out of the question.
There may come a time when I will be convinced the medical and noninvasive treatments for my angina and CAD are no longer working and I will undergo a CABG. However, I will not be coerced into what I consider to be unnecessary surgery by people I consider to be medical terrorists who are more interested in making money than properly treating my medical conditions.
Therefore, I am seeking a noninvasive cardiologist to prescribe EECP and follow me during and after the seven weeks of therapy. If you know one, please have him or her contact me at jeff.brailey@gmail.com.
Saturday, July 21, 2007
Your Angiogram Increases Your Cancer Risk
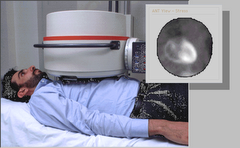
Computed tomography coronary angiography carries a "nonnegligible" risk for cancer, which varies greatly by age and gender, according to a study in JAMA.
The study was based on risk estimates -- developed for the National Academies' Biological Effects of Ionizing Radiation report -- that were applied to simulation models.
The lifetime attributable risk for cancer from a single CTCA for women was 1 in 143 at age 20, 1 in 284 at age 40, and 1 in 466 at age 60. Lung and breast cancer accounted for about 80% of the cancer risk in women.
Men's risks were considerably lower: 1 in 686 at age 20, 1 in 1007 at age 40, and 1 in 1241 at age 60. Women's higher risk was attributed to the greater radiosensitivity of their lungs and to the fact that the breast lies in the field irradiated during CTCA.
The authors note that CTCA "should be used particularly cautiously in the evaluation of young individuals, especially women."
Thursday, July 19, 2007
Choose Your Doctor Carefully
 A legal dispute involving a 69-year-old Miami heart surgeon has revealed that he has has been suspended from the staff at Cedars Medical Center while the hospital investigates 24 of his cases, which include ''numerous patient deaths,'' court filings show.
A legal dispute involving a 69-year-old Miami heart surgeon has revealed that he has has been suspended from the staff at Cedars Medical Center while the hospital investigates 24 of his cases, which include ''numerous patient deaths,'' court filings show.Other documents say the surgeon, Alex Zakharia, suffers from memory lapses that have been worsening, and he's been charged in a criminal case with fraud and perjury for allegedly exaggerating his surgical experience.
Zakharia's lawyers insist he has done nothing wrong, and the doctor has challenged his suspension. He continues to work in at least four South Florida hospitals. One week last month, he performed 21 procedures, according to court documents.
Doctors' problems are usually closely held secrets in the healthcare industry and can persist for years before becoming public with any disciplinary action.
But in this case, Zakharia's difficulties have been disclosed by the doctor's own lawyers in documents filed in Detroit and Miami-Dade County courts.
Zakharia refused to discuss any specifics and threatened to sue anyone who wrote about his situation.
In court papers, the surgeon and his lawyers have said there are no problems. The memory lapses don't affect his work, Zakharia told his doctors. He has pleaded not guilty to the fraud charges, and he has sued Cedars to be put back on staff. The lawsuit says hospital executives suspended him ``abruptly without . . . sufficient inquiry to confirm the credibility of the allegations.''
The four hospitals where he works are Mount Sinai Medical Center in Miami Beach, Select Specialty Hospital in Miami, North Shore Medical Center in North Miami-Dade and Larkin Community Hospital. Officials for Sinai, North Shore and Larkin said they didn't have any information about performance issues involving Zakharia. Select did not respond to phone calls.
According to his résumé, Zakharia received his medical degree from the American University in Beirut in 1962, followed by surgical residencies at Baylor, Case Western, the Mayo Clinic and the University of Miami. He has practiced in Miami since 1982.
START OF TROUBLES
Zakharia's present troubles stem from a 2003 case in which he testified for a man who sued the Veteran's Administration for malpractice. In November 2006, the U.S. Attorney's Office in Detroit indicted him on charges of fraud and false declaration concerning his surgical experience.
According to the indictment, he stated in a deposition that he had wide experience in coronary artery bypass graft surgeries, but records at Cedars and Miami Heart Institute didn't back up the testimony. Zakharia told The Miami Herald at the time that the lawyers had misunderstood him and that his background wasn't relevant to the malpractice case.
That same month, Cedars suspended his surgical privileges, saying in a letter to the surgeon that it had ''credible evidence'' that his surgical care in one case was ``below the standard of care.''
Several weeks later, another Cedars letter to the doctor said the medical executive committee recommended revoking his hospital privileges because of his ''clinical performance or competence'' in two other cases. Zakharia was offered a hearing to give his side.
Lourdes Garrido, spokeswoman for the HCA hospital chain, Cedars' owner, said the hospital couldn't comment because the matter is under litigation.
Zakharia sued Cedars in Miami-Dade Circuit Court to stop the hearing, alleging it was ''tainted'' because of the hospital's prejudice against him. The hearing, which has been frequently postponed, is now set for next month.
Cedars responded that it needed to ''protect the life and well-being of patients'' and that the hospital had summarily suspended him in November ``after several of his patients died.''
The court filing said that in December the Medical Executive Committee had received ``credible information regarding his clinical performance or competence concerning the deaths of two patients.''
Later, the Cedars staff said it would present 24 cases at his hearing. ''The additional 22 cases, which cover a period of 18 months, include numerous patient deaths,'' the court filing said.
Cedars said the surgeon's actions were motivated by ''ill will and animus,'' because Cedars had provided information to a federal grand jury that ended up indicting Zakharia for perjury.
NO COMMENT
Cedars lawyer Stephen Bronis said he couldn't comment because the case involves a ``confidential and privileged peer review.''
Zakharia said if an article were published about his situation, ''I am having the biggest lawsuit The Herald has ever seen. You have demeaned me'' by calling and asking questions of hospitals and others, he said. ``I am suing for $5 million. You tell your boss that.''
Zakharia's Detroit and Miami attorneys did not respond to five calls over a two-day period.
As the Cedars case grinds on, Zakharia's Detroit lawyer has filed motions seeking to get the federal perjury case moved to Miami because he was too ill to make the trip. In support, his lawyer submitted letters from doctors who have been treating him.
In one, Guillermo Blanco, a North Miami Beach neurologist, stated Zakharia suffered ''an episode of dizziness'' during one flight to Detroit for a hearing, and a magnetic resonance imaging test revealed ''two possible TIAs.'' A TIA is a transient ischemic attack, which the National Institute of Neurological Disorders and Stroke describes as a ``stroke that lasts only a few minutes.''
From Blanco's letter: 'Dr. Zakharia today complains of progressive difficulties with his memory. He has difficulty focusing on things and although he performs surgery without any difficulties, he has noted that he forgets names of patients and he has to ask his secretary frequently about it. Again he admitted not being as `sharp' as he use[d] to be. This has been going on for several months and probably longer than a year but has been worse lately.''
Blanco recommended Zakharia not fly ''because of a high risk of a stroke,'' and he recommended the surgeon take Aricept. The drug's website says it is the only drug approved ``for all stages of Alzheimer's disease.''
Carl Eisdorfer, director of UM's Center on Aging, said Aricept ''has really one specific use -- it's used in patients with Alzheimer's disease,'' but he couldn't say why Blanco prescribed it.
Blanco said he couldn't talk about a patient's medical problems.
ADVERSE EFFECTS
Another doctor treating Zakharia, Rafael A. Soto, said the surgeon had suffered during two Detroit flights, one of which ''caused heaviness in his speech. . . . While his condition does not prevent him from doing his normal professional duties, he is strongly advised not to fly.'' Soto did not respond to a phone call seeking comment.
Florida Board of Medicine records show no disciplinary actions against the surgeon. A spokeswoman said any existing investigations concerning Zakharia would not be public until the board ruled.
Zakharia remains busy. In one week last month, he did nine procedures at Mount Sinai, 10 at Select and one each at North Shore and at Larkin.
Cardiologist William O'Neill, executive dean for clinical affairs at the University of Miami's medical school, reviewed the list of procedures for The Miami Herald and said many were relatively simple -- inserting tubes into veins -- but three (one at Sinai and two at Select) were more complicated tracheotomies -- cutting open the throat to insert a ventilator tube.
While he doesn't have firsthand knowledge of the Zakharia case, each of the elements raises issues, O'Neill said.
``I would be very concerned to find out the reason he was suspended by another hospital. I would be incredibly concerned about the accusation of perjury, and I would be even more concerned about the memory issues.
``Before I let him continue at a hospital I was associated with, I'd want to know from the physical standpoint that he's mentally competent.''
Sidney M. Wolfe, a physician with the consumer group Public Citizen in Washington, said the Zakharia case is rare. Typically, physicians' problems are handled very quietly -- if they are handled at all.
Without the court cases, ''he presumably would be treated'' for his memory problems, Wolfe said, ``and no one would know the difference.''
Saturday, July 07, 2007
Number of CABG's to Increase
Three years and three months ago, I was told by a cardiologist in Indianapolis, that if I didn't undergo a quintuple coronary artery bypass within a few days, I stood a good chance of having a stroke, heart attack or being dead within three months. My heart is still ticking, it is still receiving vital oxygen and I didn't have to have my chest cracked open. I was put on a course of medication which I continue on today. If you want to know the whole story and truth, start reading this blog from the first post until the last. AND BEWARE OF NEW RELEASES LIKE THIS ONE.
New Trend Reverses Almost 5 Years of Decline
WALTHAM, Mass., June 28 /PRNewswire/ -- Millennium Research Group (MRG)has conducted a detailed analysis of the cardiac surgery market in its US
Markets for Cardiac Surgery 2007 report. The analysis reveals that there will be an increase in the number of coronary artery bypass graft (CABG)
procedures in 2007.
This marks the first time in almost 5 years that CABG procedures have increased over the previous year. The historic decline was due to the adoption and
increased popularity of less invasive methods of coronary revascularization.
These less invasive procedures have had their safety called into question over the past year.
Safety concerns of alternative procedures, combined with the increasing incidence of heart disease and demographic pressures will result in uncharacteristic CABG
procedure growth of 0.9% during 2007 and will help to support nominal growth in overall CABG procedures through 2011.
Clinical data published in late-2006 questioned the efficacy of percutaneous coronary interventions (PCI) and particularly drug-elutingstent (DES) procedures
for the treatment of certain forms of complex coronary artery disease (CAD).
Published data reported increased risk of late-stent thrombosis associated with DES implants up to a year post-operatively in patients with complex CAD including
multi-vessel or left main artery disease.
"The increase in CABG procedures in 2007 reverses a long-standingdecline," says Nadia Lachowsky, Senior Analyst at MRG. "CABG is a proven choice for many physicians
and patients. It will likely remain an importantoption for complex CAD despite technological advances in minimally invasive
treatments.
Besides CABG devices, the US Markets for Cardiac Surgery 2007 report covers markets for heart valve devices, endoscopic vessel harvesting
devices, anastomosis assist devices, cardiac assist devices (ventricular assist devices, intra-aortic balloon pump catheters, total artificial heart
devices), surgical ablation probes, and transmyocardial revascularization devices.
What this report fails to tell you is upwards to 95% of all CABG's performed in the USA are UNNECESSARY.
It fails to tell you that the CABG is one of the biggest money makers for hospitals, cardiologists and cardio-thoracic surgeons.
It fails to tell you the most prudent initial treatment of conditions like angina and CAD is medication.
BEWARE OF MEDICAL TERRORISTS WHO LIE AND TELL HALF TRUTHS TO SEPARATE YOU FROM YOUR HARD-EARNED MONEY AND PERFORM UNNECESSARY SURGERY ON YOU.
ALWAYS GET A SECOND OPINION FROM A NONINVASIVE CARDIOLOGIST.
Friday, June 15, 2007
Pennsylvania Study Protects Consumers
High death rate found in one class of operations at Altoona during 2005
A state group that tracks health care performance found a high death rate for Altoona Regional Health System and one of its surgeons for one type of heart operation in 2005.
The Pennsylvania Health Care Cost Containment Council found the higher-than-expected death rate for heart valve operations in patients who died at the hospital or within 30 days of their procedures.
The high death rate finding for the hospital was based on 59 valve operations.
The same finding for Dr. John Anastasi was based on the 50 valve operations he performed.
The hospital spoke of extenuating circumstances in a letter about the findings to the agency.
“The patients that did not fare well in the current reporting period had many complicating factors, including very advanced age, end-stage heart disease, whose only remaining option was surgery, and emergency cases performed during an acute life-threatening event,” wrote David Cowger, senior vice president of quality/medical affairs. “Many of these patients had pre-existing multi-organ disease compounding their acute cardiac care. Patient and family directives frequently limited the amount of support we could provide.”
To calculate red-flag rates, the agency uses a formula that takes into account how sick patients are.
The council also found higher-than-expected readmission rates within seven days and 30 days for the valve operations at the hospital and for those done by Anastasi.
And it found a higher-than- expected readmission rate within 30 days for the 89 coronary artery bypass graft surgeries performed by Anastasi.
The council, a quasi-governmental agency, tracks and reports performance by hospitals and in some cases individual doctors because “there is evidence that information contained in reports such as this encourages hospitals and surgeons to examine their processes and make changes that can improve quality of care and ultimately save lives,” the agency stated in its report.
Altoona constantly monitors its care to improve outcomes, Cowger wrote. All cases of “less-than-optimal outcome are reviewed,” he wrote.
The open-heart surgery team at the hospital has not had significant changes since it began in 1989, he wrote.
The 2005 report also lists Dr. Burt Fazi as performing heart surgery.
Statewide, the council found the in-hospital death rate for coronary bypass surgery patients declined in 2005, while the rates of readmission increased slightly during the same period.
The 2005 mortality rate among bypass patients was 1.9 percent, down from nearly 2 percent the previous year and from 2.4 percent in 2000.
At the same time, 5.5 percent of bypass patients were readmitted within seven days of being discharged — up from 5.2 percent — and 13.6 percent were readmitted within 30 days of being discharged, up from 13.2 percent.
Heart failure, infections and abnormal heart rhythms were the top three reasons for readmissions.
The council has published annual reports on bypass surgeries and how much hospitals charge for them since 1992. This year, it added information on heart-valve procedures, which are more invasive and complicated than bypasses, and included payment data on both procedures for the first time.
‘‘The provider community has argued for a long time that [hospital] charges do not reflect what is paid,’’ said Marc P. Volavka, the council’s executive director. ‘‘The public now has available precisely the kind of information they’re going to need.’’
UPMC was paid thousands more for cardiac surgery
But study says care, measured by deaths and readmissions, was not superior to lower-cost hospitals
A ground-breaking report released today reveals wide disparities in the amounts Pittsburgh-area hospitals received for cardiac surgeries, with the University of Pittsburgh Medical Center paid thousands more than its rivals without offering a superior level of care as measured by mortality and readmission rates.The variations are no surprise to insurers, who provided 2005 payment data for the report, produced by the Pennsylvania Health Care Cost Containment Council. And consumers are unlikely to change hospitals based on the pricing information because health plans shoulder the bulk of the cost of their care.
But one small business representative hopes the new data will motivate employers to demand a greater equality in pricing from hospital to hospital.
"If you are going to charge more, you have to show a better result," said Cliff Shannon, who represents small- and medium-sized manufacturers as president of SMC Business Councils in Churchill. "That is what we expect when we buy a car. God knows, health care is more important than the car we drive."
Referring to UPMC, the nonprofit hospital conglomerate that has major operations in Oakland, he asked: "What kind of rational decision is it to go into the city, find parking in Oakland and have the surgery cost 50 percent more? For a lot of employers, those are the questions that will echo in their heads as they think about their next health care budget."
The two highest-paid hospitals, according to the state agency that seeks to address the cost and quality of health care, were UPMC Presbyterian and UPMC Shadyside, two of 19 institutions controlled by the region's dominant medical provider and biggest employer. Together, in 2005, the East End hospitals received an average of $34,803 for coronary artery bypass graft surgery -- used on patients with significant artery blockage.
No hospital in the area received more. The average payment for the same procedure at the North Side's Allegheny General Hospital was $23,715, while at Jefferson Regional Medical Center in the South Hills, the cost was even lower: $18,009.
Yet the level of care at Jefferson Regional and Allegheny General, as measured by mortality and re-admission rates, was not inferior to that at the two UPMC facilities. In fact, Allegheny General had a lower readmission rate than its crosstown rival.
"There are dramatic differences in payment within the region that don't make a lot of sense," said Marc Volavka, executive director of the cost containment council. "Someone has to ask, 'Why'?"
The statewide report "shows that quality of care has no apparent relationship to the cost of care," said Mr. Shannon, also a board member of the cost containment council. "More expensive does not equal better; less expensive does not equal worse. How much of a premium should we have to pay to go to the brand-name hospitals in Pittsburgh when the quality of care is no better?"
The release of this report, more than a year in the making, provides greater transparency to the often-opaque discussion of rising health care costs across the region and the state
The report is unusual for including average payments made to hospitals for patients covered by commercial insurance. Past reports typically included "charges" -- the amount a hospital bills for a patient's care -- but not the final payment. Hospitals generally do not receive full reimbursement for their charges because insurers or other large purchasers negotiate discounts.
While the two UPMC hospitals had the highest commercial payment rate in the region for coronary artery bypass surgery, some hospitals elsewhere in the state were paid more.
Philadelphia's Hahnemann University, for example, had an average payment of $78,312. At the Hospital of the University of Pennsylvania, the figure was $60,733. Temple, also in Philadelphia, was paid $57,533 for the same procedure.
UPMC spokesman Wendy Zellner cited those differences as a better point of comparison, since they are all academic medical centers, like UPMC, and in that group, UPMC Presbyterian and Shadyside have the highest volume of bypass surgeries and the lowest average payment rates.
Within southwestern Pennsylvania, "various factors affect average charges and payment, including the nature and complexity of the cases that we treat," Ms. Zellner said. The growth in patient volume at UPMC "suggests that insurers and patients believe that we are providing high quality care at a fair price."
Higher prices for UPMC services were an issue last month when the state attorney general's office announced an agreement regarding the planned merger of the region's largest health system with Mercy Hospital.
State officials didn't want the merger to result in higher prices at Mercy, noting that they are currently lower than at UPMC. Health system officials agreed to extend existing health plan contracts at Mercy and their pricing for eight years, with allowances for inflation. Before it could take place, the merger also would need approval from the Federal Trade Commission and the Vatican.
At Mercy, the average payment for a coronary artery bypass was $25,315 -- almost $10,000 less than at the two UPMC facilities (but more than the $24,834 paid to UPMC Passavant, a community hospital in the North Hills). "I don't know if I can explain that great discrepancy," said Dr. Ross DiMarco Jr., chief of cardiovascular and thoracic surgery at Mercy.
West Penn Allegheny Health System, parent of the West Penn Hospital and Allegheny General, raised the same question yesterday, noting that its hospitals performed "on par or better" than the two UPMC hospitals in the East End and still UPMC is paid more.
"In any other market, quality and efficiency are rewarded," said Tom Chakurda, spokesman for West Penn Allegheny. "That does not appear to be the case in health care."
Despite the variation in payment, mortality and hospital readmission rates at local hospitals were generally what would be expected for bypass and valve surgeries, according to the cost containment council report. Some facilities, including Allegheny General, St. Clair Memorial and The Medical Center, Beaver, had lower-than-expected rates for some surgeries. Washington and Westmoreland Regional hospitals, however, had some that were higher than expected.
For a variety of reasons, large medical centers are able to negotiate higher payment rates from insurers or other purchasers, said Dr. Carey Vinson, vice president for quality and medical performance management at Highmark.
The medical care they provide, along with teaching and research, represent "a unique set of services to the community," Dr. Vinson said. "They parlay that into asking for greater reimbursement."
Large centers also contend they treat more complex needs and have higher costs, he said.
But smaller hospitals also try to strengthen their negotiating position -- for example, by noting if they are the only medical facility in a particular area, Dr. Vinson said.
"All hospitals try to leverage their uniqueness when they can," he said.
Medicare payment rates for the cardiac surgeries also varied, according to the report. Medicare officials noted that those rates can be affected by a number of factors, including whether hospitals are teaching facilities or serve large numbers of poor patients.
The report also noted that mortality rates, lengths of stay and payments were much higher when patients having the cardiac surgeries acquired infections in the hospital.
Jessica Seabury, executive director of the Consumer Health Coalition, said payment incentives are needed that better promote good care. Her group works to increase access to quality, affordable health care in southwestern Pennsylvania.
Carolyn Scanlan, president of the Hospital & Healthsystem Association of Pennsylvania, the hospital industry's main lobby in the state, noted that the report indicates that in-hospital mortality rates for cardiac bypass surgeries have continued to drop. She said more study is needed concerning the payment data and information on hospital-acquired infections and lengths of stay.
Wednesday, June 13, 2007
Maltreatment of Black Medicare Patients
The study used recent data to confirm and update knowledge of racial disparities persisting in the health care system.
"We found some significant differences, and definitely, we have no good explanation for why," said lead researcher Dr. Ioana Popescu, health services researcher at Iowa City VA Medical Center. "More research needs to be done."
The study is published in the June 13 issue of the Journal of the American Medical Association.
"This study uses a contemporary cohort, following patients through 2005, and this is the first study to look at that," said Popescu, who is also a junior faculty member at the University of Iowa Carver College of Medicine in Iowa City.
The study also differs from previous research in that it stratifies patients by hospital type, meaning those that do and do not provide specialized heart services.
Prior studies have indicated that racial differences in care after a heart attack appear most pronounced when it comes to invasive and costly technologies such as coronary revascularization or procedures to get the blood flowing again to the heart.
The most common type of revascularization is coronary artery bypass graft (CABG).
Some recent studies have suggested that differing access to high-quality providers might account for some racial disparities.
Less than one-fifth of U.S. acute-care hospitals provide coronary revascularization, and many Medicare beneficiaries are initially admitted to hospitals that don't provide CABG or percutaneous coronary intervention (PCI, formerly known as angioplasty).
Few studies have looked at such patterns of care and how they might impact disparities.
For this study, the authors looked at more than 1.2 million black and white Medicare beneficiaries aged 68 and older who had been admitted to one of 4,627 U.S. hospitals between 2000 and 2005 with a heart attack. The hospitals were mixed, some having revascularization services and some not.
Black patients admitted to hospitals with or without revascularization services were less likely to undergo revascularization than white patients (34.3 percent vs. 50.2 percent and 18.3 percent vs. 25.9 percent) and were also more likely to die within one year (35.3 percent vs. 30.2 percent and 39.7 percent vs. 37.6 percent).
In addition, black patients admitted to hospitals without these specialized services were less likely to be transferred to a hospital with the services within two days (7.4 percent versus 11.5 percent) and within 30 days (25.2 percent versus 31 percent) of admission.
The likelihood that a black patient admitted to a hospital without revascularization services would be transferred was also 22 percent lower than their white counterparts, the team found.
Even among patients who were transferred, blacks were 23 percent less likely to undergo revascularization.
Blacks had a 9 percent lower risk of death during the first 30 days after admission to the hospitals with revascularization services and 10 percent lower in the other hospitals. Between 30 days and one year after admission, blacks had a 12 percent to 26 percent higher risk of death. The risks were lower if the patient underwent revascularization but were still higher than for whites.
Some aspects of the data were unclear, however, including what type of heart attack the participants suffered. The guidelines for revascularization can be different depending on the characteristics of the heart attack, noted Dr. John P. Erwin III, associate professor of internal medicine at Texas A&M Health Science Center College of Medicine and cardiologist at Scott & White Hospital in Temple.
It's also unclear why such disparities exist.
"Probably we should look at other potential contributors to the differences that we notice such as more clinical information on patients," Popescu said. "There may be some underlying baseline differences such as symptoms in the beginning, the time they chose to come to the hospital, which may play role in getting the procedure and the diagnosis. Definitely we need more research into patient preferences and decision-making."
"Aspects of medical decision-making were unclear," Erwin added. "More data points would have helped us understand it."
For Dr. John Underwood, a cardiologist in Scottsdale, Ariz., and past president of the Association of Black Cardiologists, the findings confirm previous patterns seen in medicine. And if patients aren't undergoing procedures such as revascularization, then they're less likely to be followed up.
"You're not tied into the system, those things aren't happening, and people are dying," he said.
CABG may adveresly affect brain function
Researchers at Johns Hopkins School of Medicine in Baltimore assessed 15 patients, age 57 to 81, who underwent coronary artery bypass graft surgery and were believed to be at high risk for postoperative stroke.
All 15 patients took the Mini-Mental Status Examination before surgery, which measures thinking, learning, and memory. Their mean arterial blood pressure, or MAP, which estimates the pressure of the blood that perfuses the organs of the body, was taken before and during surgery. Thirteen patients also underwent postoperative magnetic resonance imaging of their brains.
The researchers found that patients whose MAP decreased by 27 millimeters or mercury or more during surgery scored significantly lower on the Mini-Mental Status Examination after surgery.
The team also found that six of the 13 people who underwent MRIs had evidence of acute strokes, and those who had the 27-plus millimeter drop in MAP were 2.7 times as likely to have such a lesion as those whose MAP decreased by a smaller amount.
The researchers said the cognitive declines they noted might be partially due to the strokes, and proposed further studies to define the relationship between operative MAP drop, stroke and poorer short-term postoperative cognitive performance.
A report on the research appears in the early online edition of the August issue of Archives of Neurology.
Tuesday, June 05, 2007
Don't be deceived
Cardiac Surgery Death Rates Decline To Lowest Level In A Decade
Check this story out and remember: THE NUMBER OF CABG OPERATIONS BEING PERFORMED IS DECREASING BECAUSE PATIENTS AND RESEARCHERS ARE ON TO THE LIE THAT IT IS THE TREATMENT OF CHOICE FOR CAD. IT IS NOT!Cardiac Surgery Death Rates
Cardiac surgery death rates have dropped to their lowest level since the New Jersey Department of Health and Senior Services began issuing reports a decade ago.
The state's mortality rate has declined 54.5 percent between 1994 and 2004, including a nearly 12 percent drop from 2003 to 2004, according to the report.
"The cardiac surgery reporting initiative is a real success story. It shows what a powerful difference we can make when we work together with one goal in mind -- giving every patient high-quality care," Commissioner Jacobs said.
"Cardiac surgery programs have succeeded because of their remarkable efforts to examine the care they give and make systematic improvements," said Charles Dennis, M.D., chairman of the Commissioner's Cardiovascular Health Advisory Panel. "I appreciate the Department's ongoing support for the panel's efforts to track and report on patient outcomes."
The Cardiac Surgery in New Jersey series focuses on a common cardiac surgical procedure – coronary artery bypass graft (CABG) surgery with no other major surgery during the same hospital admission.
Included in the report are patient mortality data for New Jersey's 17 cardiac surgery hospitals and 49 individual named surgeons. For the first time, the report also includes each hospital's average length of patient stay following surgery.
According to the report released today, the number of CABG surgeries continues to decline as patients are increasingly treated with angioplasty, a less invasive alternative to bypass surgery. There were 6,177 procedures in 2004 compared with a high of 8,377 in 1998. ( How many were treated medically in those years?)
Of the 6,177 patients, 122 -- or 1.98 percent -- died in the hospital or within 30 days of surgery. (How many patients treated with medication died in the first 30 days of treatment?) In 1994-1995, the period covered by the first report, the rate was 4.14 percent. The department risk-adjusts all hospital and surgeon rates to, in effect, give "extra credit" to those treating sicker patients.
Other hospital findings include:
* Hackensack University Medical Center was the only hospital with a statistically significantly better-than-average performance (0.65 percent death rate).
* Our Lady of Lourdes Medical Center in Camden (4.46 percent) and the UMDNJ-University Medical Center in Newark (6.84 percent) had rates that were significantly worse than the statewide average.
* Englewood Hospital and Medical Center had no deaths among its 102 patients, but the rate was not statistically significantly different from the state average.
* The statewide average patient stay in the hospital was 6.43 days, with individual hospitals ranging from 5.64 to 7.39 days.
Jersey City Medical Center received its cardiac surgery license in late 2004 and will be included in the next report.
The 49 surgeons named in the report had performed at least 100 bypass operations in one hospital in the years 2003-2004 combined. That is the minimum number needed to calculate reliable risk-adjusted mortality rates. Surgeon findings include:
* Three surgeons had a statistically significantly better-than-average performance – one each at Hackensack University Medical Center, AtlantiCare Regional Medical Center and St. Michael's Medical Center.
* Three had worse than average performances – one each at Cooper Hospital/University Medical Center, Our Lady of Lourdes Medical Center and PBI Regional Medical Center.
* One surgeon each at Englewood Hospital and Medical Center and Newark Beth Israel Medical Center had no deaths, although this was not statistically significantly different from the statewide average.
Four other states report on cardiac surgery outcomes. Pennsylvania and Massachusetts also examine 30-day mortality, while New York and California look at in-hospital deaths.
FDA Warns on Chinese-Manufactured Toothpaste
The FDA is warning consumers to throw out any Chinese toothpaste after it found a component of antifreeze in several products.
Because diethylene glycol (DEG) is not always listed in the ingredients on the package, the FDA says people should examine their toothpaste and discard any imported from China. So far there have been no reports of injuries from DEG-contaminated toothpaste, but there have been deaths in several countries from DEG-contaminated products like cough syrup. The FDA is concerned about chronic exposure to DEG, particularly to vulnerable populations like children and people with kidney or liver disease.
The following brands are affected by the advisory: Cooldent Fluoride, Cooldent Spearmint, Cooldent ICE, Dr. Cool, Everfresh, Superdent, Clean Rite, Oralmax Extreme, Oral Bright Fresh Spearmint Flavor, Bright Max Peppermint Flavor, ShiR Fresh Mint Fluoride Paste, DentaPro, DentaKleen, and DentaKleen Junior.
Link(s):
FDA advisory (Free) http://click2.nejm.org/cts
Wednesday, May 02, 2007
Canadian Women Get Sicker From Coronary Disease
During seven years of not feeling well, Silvia Rizzuto never thought about her heart.
The middle-aged mother of two chalked up her fatigue, her shortness of breath, to stress and being overweight.
Then she got sicker – constantly feeling tired, occasionally blanking out for a second – and her doctor finally referred her to a cardiologist.
Her life was more imperiled than she ever realized. While undergoing tests, Rizzuto suffered cardiac arrest.
She was revived and diagnosed with ventricular tachycardia, a rapid heart beat that can cause sudden cardiac death – she had a defibrillator implanted in her chest. Rizutto also had hypertrophic obstructive cardiomyopathy – part of her heart had thickened, impeding blood flow. Last June she underwent more than four hours of open-heart surgery to carve away part of the thickened muscle.
"I always worried about breast cancer and carefully checked myself," says Rizzuto, 49. "I knew nothing about heart disease. It came as a very big shock."
Cardiologists hear this from women all the time. But more Canadian women die every year from cardiovascular disease – 36,695 deaths in 2004 – than from all the cancers combined: 32,458 women were claimed by cancers in 2004. The news gets worse. For the first time, cardiovascular disease is now an equal opportunity killer, felling nearly as many women as men, according to a report this year from the Heart and Stroke Foundation of Canada. The report also pointed to an alarming gender gap: women are less likely than men to receive the right treatment and more likely to die. It has prompted Heart and Stroke to explore a national campaign to highlight women and heart disease, modeled after a successful six-year awareness blitz in the U.S.
"We need to do a better job marketing the impact of cardiovascular disease in women," says Heather Ross, medical director of cardiac transplants at Toronto General Hospital. "It's absolutely a hot topic."
The topic earned headlines last month when Canadian singer Jann Arden was hospitalized with takotsubo, or stress-induced cardiomyopathy – also known as broken heart syndrome. The disorder, believed to be more prevalent in women, may first appear with sudden chest pain, and causes part of the heart to bulge.
Last month, the Canadian Medical Association Journal devoted a special supplement to sex-specific issues related to cardiovascular disease. "We've summarized what's known and identified the knowledge gaps," says Louise Pilote, principal investigator on GENESIS, a five-year project involving 40 Canadian researchers studying sex and gender factors of heart disease and stroke.
One key knowledge gap: Doctors can't fully explain why the incidence and mortality of heart disease and stroke is decreasing among men and not women.
"Female patients are slightly older and sicker," says Toronto cardiologist Beth Abramson, "but even when you correct for age, it doesn't explain it."
Women's hearts tend to be protected before menopause, possibly through the effects of estrogen. After menopause, their risk of heart disease and stroke rises. The average age for a heart attack in women is 65, compared to 55 for men.
The misconception that cardiac disease is a man's problem is a bias held by both patients and some medical professionals, says Leonard Sternberg, director of cardiology at Women's College Hospital. "Women need to be more pro-active about their hearts."
That gender bias could keep a woman's heart disease from being diagnosed early – or even prevented. There's even been confusion about the signs of a female heart attack. Doctors used to believe women presented different symptoms than men, but now that's doubted, according to cardiologist Abramson, spokesperson for the Heart and Stroke Foundation. "Women may just describe the symptoms differently," she says.
While about 70 per cent of heart attacks cause chest pain in both male and female victim, 30 per cent do not, says cardiologist Sharonne Hayes, director of the Women's Heart Clinic at the Mayo Clinic in Rochester, Minn. Instead, they experience a mix of symptoms – shortness of breath, gastrointestinal upset, loss of consciousness, excessive sweating.
Women are also less likely to be treated by a cardiologist or receive coronary artery bypass graft surgey or angioplasty (to reopen blocked arteries) than men, according to the recent Heart and Stroke Foundation report.
"The advances in the treatment of cardiovascular diseases have been fairly dramatic," says Hayes. "If you're not seeing a specialist, you're not being offered the treatment you're eligible for."
Another hurdle for women has been their low numbers in cardiovascular clinical trials, at about only 20 per cent, says cardiologist Ross, even though women account for 62 percent of deaths by heart failure. The disease is more common in the elderly, and that means women since human females outlive males.
Scientists don't yet fully understand what biological gender differences might affect heart disease and treatment. "We're on the cusp of learning a whole lot more, of better understanding the role of hormones," says Hayes.
For example, the HRT results of the landmark Women's Health Initiative Study surprised the world's medical community in 2002. Once thought to protect post-menopausal women from cardiovascular disease, hormone replacement therapy appeared, instead, to be linked to increased risk of heart disease and stroke.
In her animal research, Carin Wittnich, director of the cardiovascular sciences collaborative program at UofT, has found that estrogen is a "double-edged sword."While it helps protect healthy female hearts, estrogen may hurt a diseased heart before menopause. "It's not straightforward," says Wittnich. "We're slowly peeling each layer, like an onion."
What is more straightforward is how to keep a heart healthy. The majority of cardiovascular disease cases could be prevented, says the Mayo Clinic's Hayes. Notwithstanding family history, people can control risk factors such as high blood pressure and cholesterol, smoking, obesity and a sedentary lifestyle. Diabetes is of particular concern: It increases the chances of cardiovascular disease by 70 per cent in women, compared to 40 per cent in men, says TGH cardiologist Ross.
Heart patient Rizzuto changed her attitude, with the help of the cardiac rehabilitation program at Women's College. "It made me realize I need to take time for myself," says Rizzuto. "Before it was always about family, never me."
The rehab program, which includes educational sessions and personal support, is the sole women-only program in North America, says Jennifer Price, nurse practitioner in cardiology at Women's College. Rizzuto works out on the hospital's exercise equipment twice weekly and meets with a dietician about weight loss. She's joined a fitness centre to keep exercising when her six months in rehab ends. She's also enjoying long walks in her neighbourhood. "I'm definitely more energetic," smiles Rizzuto, using the step machine. "I feel alive now."
From the Toronto Star