Saturday, February 23, 2008
Medications & Supplements
I have been asked to list the medications and supplements I take daily. While all of them are not for the hypertension/coronary artery disease this blog addresses, they all have a purpose in my plan for overall health.
First,, let me list the prescribed drugs:
Metoprolol Tartrate - 100mg 7 am and 7 pm - for blood pressure
Fosinopril Sodium - 10mg 7 pm - for blood pressure
Isosorbide Dinitrate - 5mg 7 am, 10mg 1 pm, 15mg 7 pm - for blood pressure
Budeprion XL - 300mg 7 am - mood elevator
Carbidopa/Levodopa - 25/100mg - Parkinson's disease
Rotigotine Transdermal System - 6mg/24hrs - Parkinson's disease
Over-the-counter medications & supplements
Aspirin - 325mg 7 am - anticoagulant
Prilosec OTC 20mg 7pm prn - heartburn
Vitamin C - 1000mg 1 pm and 7 pm - antioxidant
Omega 3 Fish Oil - 1200mg 7 am 1 pm 7 pm - help prevent heart disease/high blood pressure
Coenzyme Q-10 - 120mg 7 pm - antioxidant
Vitamin E - 400IU 7 pm - antioxidant
L-Carnitine - 250mg 7 am - helps disposal of fat.
L-Arginine - 500mg 7 am - Inhibits nitrous oxide reaction
Vitamin B Complex 100mg each 7 am - cell metabolism, enhance immune system, promote cell growth.
Glucosamine/Chondroitin/MSM - 1500mg/1200mg/500mg 7am, 1pm, 7pm - Nourishes cartiledge and connective tissues maintaining integrity of the joint, assists in wound healing, strengthens collagen fiber, reduces osteoarthritis pain.
Folic Acid - 800mcg 1 pm - prevent anemia, healthy red blood cells
Selenium - 200mcg 7 am 7 pm - thyroid health
Lysine - 500mg 7 am, 1pm, 7 pm - an essential amino acid
There you have it. My daily regimen of medications and supplements. As with any medication and supplement, people should discuss the implementation of this or a similar regimen with their physician before starting it.
First,, let me list the prescribed drugs:
Metoprolol Tartrate - 100mg 7 am and 7 pm - for blood pressure
Fosinopril Sodium - 10mg 7 pm - for blood pressure
Isosorbide Dinitrate - 5mg 7 am, 10mg 1 pm, 15mg 7 pm - for blood pressure
Budeprion XL - 300mg 7 am - mood elevator
Carbidopa/Levodopa - 25/100mg - Parkinson's disease
Rotigotine Transdermal System - 6mg/24hrs - Parkinson's disease
Over-the-counter medications & supplements
Aspirin - 325mg 7 am - anticoagulant
Prilosec OTC 20mg 7pm prn - heartburn
Vitamin C - 1000mg 1 pm and 7 pm - antioxidant
Omega 3 Fish Oil - 1200mg 7 am 1 pm 7 pm - help prevent heart disease/high blood pressure
Coenzyme Q-10 - 120mg 7 pm - antioxidant
Vitamin E - 400IU 7 pm - antioxidant
L-Carnitine - 250mg 7 am - helps disposal of fat.
L-Arginine - 500mg 7 am - Inhibits nitrous oxide reaction
Vitamin B Complex 100mg each 7 am - cell metabolism, enhance immune system, promote cell growth.
Glucosamine/Chondroitin/MSM - 1500mg/1200mg/500mg 7am, 1pm, 7pm - Nourishes cartiledge and connective tissues maintaining integrity of the joint, assists in wound healing, strengthens collagen fiber, reduces osteoarthritis pain.
Folic Acid - 800mcg 1 pm - prevent anemia, healthy red blood cells
Selenium - 200mcg 7 am 7 pm - thyroid health
Lysine - 500mg 7 am, 1pm, 7 pm - an essential amino acid
There you have it. My daily regimen of medications and supplements. As with any medication and supplement, people should discuss the implementation of this or a similar regimen with their physician before starting it.
Friday, February 22, 2008
Update #5
I continue to be free of angina pain after once again dodging the knife of the cardio-thoracic surgeon. Just to bring you up to date, I once again opted to treat my coronary artery disease medically rather than through bypass surgery. My faith still lies with my former cardiologist, Howard Wayne, who explained angiogenesis and the collateral vessel system to me back in 2004, when I sought a second opinion from him.
Since the addition of Isordil to my medication regimen, my blood pressure fluctuates between 128/72 and 96/55. The lower blood pressures are always obtained in the evening. I would like my BP to become approximately 90/50 at all times when I am at rest. That should control the hypertension I was experiencing when I was under physical or emotional stress.
The good news is that I have not had an angina attack since the one that sent me to the emergency room of the Indiana Heart Hospital last month.
Since the addition of Isordil to my medication regimen, my blood pressure fluctuates between 128/72 and 96/55. The lower blood pressures are always obtained in the evening. I would like my BP to become approximately 90/50 at all times when I am at rest. That should control the hypertension I was experiencing when I was under physical or emotional stress.
The good news is that I have not had an angina attack since the one that sent me to the emergency room of the Indiana Heart Hospital last month.
Labels:
angina,
bypass,
cabg,
coronary artery disease,
hypertension,
Isordil
Saturday, February 16, 2008
Update #4
This entry in my blog contains some references to sexual activity. If you find this embarrassing, please read no further. Also, patients on nitrates are advised to consult their cardiologist before attempting what you read here.
Valentine's Day came and went and my vital signs stayed pretty much the same as they had the day before. The Isordil has not lowered the blood pressure to anywhere the 90/50 level that I maintained it at from 2004 to 2006. I am somewhat disappointed at the progress but will maintain my dosages at 5/10/15mg at 7 am, 1 pm and 7 pm.
On February 15, I did try something different. Anticipating the opportunity for intimate activities with my significant-other, I decided to forgo the 7 pm dose of Isordil and to take 20mg of Levitra at 8:00 pm instead. Now I realize all the furor that occurred when Viagra was blamed for the heart attacks of some men who took it shortly after approval by the FDA. The warning that this drug could cause low blood pressure and heart attacks was added to Viagra, Cialis and Levitra.
The correlation between these drugs and heart attacks is a very tenuous one as far as I am concerned. In my humble layman's opinion, the fact that they also lower the blood pressure can be taken into consideration by the person on nitrates and these drugs can be adjusted accordingly. As I said above, I did not take my 15mg dose of Isordil at 7 pm and popped a 20mg tablet of Levitra at 8 pm.
I felt no untoward side effects. My blood pressure did drop significantly by 10 pm however. It went from 116/62 with a 68 pulse at 6 pm to 88/46 with a pulse of 72 at 10 pm. It should be noted, the 88/46 is about what I want my BP to register at rest all of the time.
My significant-other and I engaged in intimate sexual activities for approximately an hour and then rested. By 1 am, my blood pressure was 112/56 and the pulse was 68. We then went to sleep, waking at approximately 6 am for another session of intimate activities which lasted about a half hour. There were no negative side effects and I felt absolutely no angina during these two sessions.
Given the drop in blood pressure that followed ingestion of the 20mg of Levitra, perhaps this drug should be used to control blood pressure as well as treat erectile dysfunction. I would be interested in hearing from cardiologists what they think about this Levitra experiment I conducted last night. Also, if you are a patient on nitrates, I would be curious if you have had any experience taking one of these drugs.
I am not suggesting that anyone on nitrates attempt to do what I did last night without first seeking the advice of competent medical authority. I did and received two totally different answers. One physician told me to definitely not do it. The other said, "Go ahead and try it, you never follow my advice anyway."
Again, let me reiterate that I believe the correlation between nitrates and drugs that treat erectile dysfunction has not been properly studied. In my opinion, it is like saying since 50% of the men who had a heart attack ate red meat within 24 hours of their cardiac event that the meat was the cause of their heart attack. I will admit the drop in blood pressure could be troublesome, particularly if the person has never maintained their blood pressure at rest that low.
Valentine's Day came and went and my vital signs stayed pretty much the same as they had the day before. The Isordil has not lowered the blood pressure to anywhere the 90/50 level that I maintained it at from 2004 to 2006. I am somewhat disappointed at the progress but will maintain my dosages at 5/10/15mg at 7 am, 1 pm and 7 pm.
On February 15, I did try something different. Anticipating the opportunity for intimate activities with my significant-other, I decided to forgo the 7 pm dose of Isordil and to take 20mg of Levitra at 8:00 pm instead. Now I realize all the furor that occurred when Viagra was blamed for the heart attacks of some men who took it shortly after approval by the FDA. The warning that this drug could cause low blood pressure and heart attacks was added to Viagra, Cialis and Levitra.
The correlation between these drugs and heart attacks is a very tenuous one as far as I am concerned. In my humble layman's opinion, the fact that they also lower the blood pressure can be taken into consideration by the person on nitrates and these drugs can be adjusted accordingly. As I said above, I did not take my 15mg dose of Isordil at 7 pm and popped a 20mg tablet of Levitra at 8 pm.
I felt no untoward side effects. My blood pressure did drop significantly by 10 pm however. It went from 116/62 with a 68 pulse at 6 pm to 88/46 with a pulse of 72 at 10 pm. It should be noted, the 88/46 is about what I want my BP to register at rest all of the time.
My significant-other and I engaged in intimate sexual activities for approximately an hour and then rested. By 1 am, my blood pressure was 112/56 and the pulse was 68. We then went to sleep, waking at approximately 6 am for another session of intimate activities which lasted about a half hour. There were no negative side effects and I felt absolutely no angina during these two sessions.
Given the drop in blood pressure that followed ingestion of the 20mg of Levitra, perhaps this drug should be used to control blood pressure as well as treat erectile dysfunction. I would be interested in hearing from cardiologists what they think about this Levitra experiment I conducted last night. Also, if you are a patient on nitrates, I would be curious if you have had any experience taking one of these drugs.
I am not suggesting that anyone on nitrates attempt to do what I did last night without first seeking the advice of competent medical authority. I did and received two totally different answers. One physician told me to definitely not do it. The other said, "Go ahead and try it, you never follow my advice anyway."
Again, let me reiterate that I believe the correlation between nitrates and drugs that treat erectile dysfunction has not been properly studied. In my opinion, it is like saying since 50% of the men who had a heart attack ate red meat within 24 hours of their cardiac event that the meat was the cause of their heart attack. I will admit the drop in blood pressure could be troublesome, particularly if the person has never maintained their blood pressure at rest that low.
Wednesday, February 13, 2008
Update #3
I continue angina free, despite getting supplies of wood from outside to keep our wood stove burning. Today's vital signs are as follows:
02/13/08 - 0800 hrs - 112/64 - 68
02/13/08 - 1400 hrs - 109/59 - 70
02/13/08 - 2000 hrs - 108/60 - 64
02/13/08 - 0800 hrs - 112/64 - 68
02/13/08 - 1400 hrs - 109/59 - 70
02/13/08 - 2000 hrs - 108/60 - 64
Tuesday, February 12, 2008
Update #2
My blood pressure has yet to get to the level it was when I started Dr. Wayne's medication regimen. I am going to continue with current dosages for the remainder of the month then will increase to 10mg at 7 am, 20mg at 1 pm and 30mg at 7 pm.
o2/11/08 - 0800 hrs - 124/70 - 70
02/11/08 - 1400 hrs - 120/64 - 68
02/11/08 - 2000 hrs - 116/60 - 64
This morning's reading at 0720 hrs was 112/64 and the pulse was 63. I continue to be free of angina and there are no side effects that I can feel.
o2/11/08 - 0800 hrs - 124/70 - 70
02/11/08 - 1400 hrs - 120/64 - 68
02/11/08 - 2000 hrs - 116/60 - 64
This morning's reading at 0720 hrs was 112/64 and the pulse was 63. I continue to be free of angina and there are no side effects that I can feel.
Sunday, February 10, 2008
Update #1
I began taking the Isordil the evening of February 7. My dosage schedule is as follows: 7 am - 5mg, 1 pm - 10mg, 7 pm - 15mg. I have had no angina since beginning the Isordil. My blood pressures and pulse are as follows:
02/07/08 - 2000 hrs - 134/83, 86
02/08/08 - 1400 hrs - 136/85, 72
02/08/08 - 2200 hrs - 138/90, 90
02/09/08 - 1200 hrs - 139/79, 64
02/09/08 - 1500 hrs - 143/80, 68
02/09/08 - 2400 hrs - 106/55, 70
02/10/08 - 1200 hrs - 110/58, 78
02/07/08 - 2000 hrs - 134/83, 86
02/08/08 - 1400 hrs - 136/85, 72
02/08/08 - 2200 hrs - 138/90, 90
02/09/08 - 1200 hrs - 139/79, 64
02/09/08 - 1500 hrs - 143/80, 68
02/09/08 - 2400 hrs - 106/55, 70
02/10/08 - 1200 hrs - 110/58, 78
Thursday, February 07, 2008
Isodil Update
On Monday I turned in my Isodil prescription to the pharmacist and learned the pharmaceutical company no longer makes that brand of drug. Since the doctor did not allow substitution and only generic drugs were available, the pharmacy called the cardiologist to get permission to substitute. By Tuesday the problem had not been resolved but the pharmacy technician said she would check with the doctor again. The doctor okayed the substitution on Wednesday but the pharmacy didn't have any generic drug in stock. Finally, this morning the drug is in. I plan on starting it tomorrow morning.
My blood pressure is averaging 110/68. I want to try to get the systolic below 100 and the diastolic below 60. I will start recording my pulse and blood pressure on the blog daily when I begin the new medication.
My blood pressure is averaging 110/68. I want to try to get the systolic below 100 and the diastolic below 60. I will start recording my pulse and blood pressure on the blog daily when I begin the new medication.
Tuesday, February 05, 2008
Most Physicians Don't Understand
I saw my primary care physician yesterday.In the past, she was very supportive of my desire to maintain control of my medical treatment plan. She is an osteopath by training and very open to alternative treatments. But yesterday, she asked me why I did not have stents put in when I had the angiogram last Thursday. I told her that the purpose for the angiogram was to compare it with the one done four years earlier. I specifically crossed out the possibility of performing angioplasty, inserting stents or performing bypass surgery on the consent form I signed. As far as I was concerned, and the cardiolgist performing the cardiac catheterization agreed, this procedure was being performed strictly for diagnostic and comparison reasons.
Another reason I saw my PCP yesterday was to ask her for a prescription for Moduretic. My cardiologist refused to provide one because he said it wasn't indicated. My PCP didn't write one because she is unfamiliar with this diuretic.
This may be an appropriate place to discuss Dr. Howard Wayne's rationale for using diuretics in his treatment of hypertension and coronary artery disease. Here are the good doctor's own words, taken from his last book, Do You Really Need Bypass Surgery? A Second Opinion. It is available at http://www.heartprotect.com.
Moduretic is a combined thiazide and potassium blocker. The generic name is hydrochlorothiazide and amiloride. Amiloride is a potassium sparing agent and is in an amount of 5 mg per tablet. The HCTZ in each tablet is 50 mg. The usual dosage of Moduretic is one 5/50mg tablet twice daily.
Another reason I saw my PCP yesterday was to ask her for a prescription for Moduretic. My cardiologist refused to provide one because he said it wasn't indicated. My PCP didn't write one because she is unfamiliar with this diuretic.
This may be an appropriate place to discuss Dr. Howard Wayne's rationale for using diuretics in his treatment of hypertension and coronary artery disease. Here are the good doctor's own words, taken from his last book, Do You Really Need Bypass Surgery? A Second Opinion. It is available at http://www.heartprotect.com.
DIURETICS
"One of the most important classes of drugs I recommend in the treatment of coronary artery disease is diuretics... Most cardiologists do not use this class of drugs in the treatment of this disease. Indeed, most cardiologists don't use diuretics in the treatment of hypertension even though the Joint National Committee on Hypertension has officially been recommending for years that diuretics along with beta blockers be the first two drugs used.
"Diuretics remove excess fluid from the body by increasing the excretion of sodium and water by the kidneys. This is followed by a reduction of the volume of blood circulating within the blood vessels throughout the body. This leads to dilatation of the small blood vessels which lowers the resistance to the flow of blood. The result is a fall in blood pressure.
"Unfortunately, many cardiologists are reluctant to use diuretics in the treatment of both coronary artery disease and hypertension. This was the result of many years of misinformation that diuretics were actually harmful because they temporarily induced certain metabolic changes such as elevation of creatinine, cholesterol, triglycerides, blood sugra, calcium and uric acid, and caused a loss of potassium. Unfortunately the complications of undertreatment of hypertension and coronary artery disease caused for more problems than minor changes in the blood chemistries. Indeed, the metabolic changes that supposedly occurred following the administration of diuretics disappeared within a few months of continued usage and the addition of supplementary potassium medication."
"Diuretics remove excess fluid from the body by increasing the excretion of sodium and water by the kidneys. This is followed by a reduction of the volume of blood circulating within the blood vessels throughout the body. This leads to dilatation of the small blood vessels which lowers the resistance to the flow of blood. The result is a fall in blood pressure.
"Unfortunately, many cardiologists are reluctant to use diuretics in the treatment of both coronary artery disease and hypertension. This was the result of many years of misinformation that diuretics were actually harmful because they temporarily induced certain metabolic changes such as elevation of creatinine, cholesterol, triglycerides, blood sugra, calcium and uric acid, and caused a loss of potassium. Unfortunately the complications of undertreatment of hypertension and coronary artery disease caused for more problems than minor changes in the blood chemistries. Indeed, the metabolic changes that supposedly occurred following the administration of diuretics disappeared within a few months of continued usage and the addition of supplementary potassium medication."
Moduretic is a combined thiazide and potassium blocker. The generic name is hydrochlorothiazide and amiloride. Amiloride is a potassium sparing agent and is in an amount of 5 mg per tablet. The HCTZ in each tablet is 50 mg. The usual dosage of Moduretic is one 5/50mg tablet twice daily.
Monday, February 04, 2008
Second Verse, Same as the First
My cardiologist highly encouraged me to undergo a coronary artery bypass today. He said that I was a good candidate for the surgery because my heart is still in great shape. The post-angiogram diagnosis showed "severe three vessel obstructive coronary artery disease. Norma LV systolic function with an ejection fraction of 60%. Mildly elevated LVEDP 15mmHg."
The angiogram report stated :
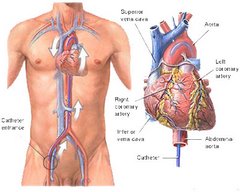
LAD: "The LAD (left anterior descending) artery is a large vessel in its proximal segment and then tapers in it mid-segment to a long region of diffuse 80-90% disease. A moderate-sized first diagonal is present with an 80% proximal stenosis. The apical LAD is large enough for bypass grafting."
Circumflex: "The circumflex is a moderate-sized vessel that supplies a moderate-sized OM-1, a moderate-sized branching OM-2 and a moderate-sized posterolateral. A 99% subtotal lesion is present in the ostial/proximal OM-1. A subtotal bifurcation lesion is present atthe junction of the OM-2 and posterolateral and extends into the proximal OM-1 and into the continuation of the circumflex."
RCA: The RCA (right coronary artery) is a large dominant ectatic vessel that supplies a moderate-sized PDA (posterior descending artery) and a moderately-sized posterolateral branch. A 90% proximal RCA stenosis is present. A 90% proximal RCA stenosis is present. A 95% stenosis of the proximal PDA is present. A 95% stenosis of the mid-portion of the posterolateral is present."
Hemodynamics: "Hemodynamic assessment demonstrates no systemic hypertension and mildly elevated LVEDP 15 mmHg."
Coronary Circulation: "Left Main:Normal. The LAD (left anterior descending) artery is a large vessel in its proximal segment and then tapers in it mid-segment to a long region of diffuse 80-90% disease. A moderate-sized first diagonal is present with an 80% proximal stenosis. The apicala LAD is large enough for bypass grafting. Circumflex: The circumflex is a moderate-sized vessel that supplies a moderate-sized OM-1, a moderate-sized branching OM-2 and a moderate-sized posterolateral. A 99% subtotal lesion is present in the ostial/proximal OM-1. A subtotal bifurcation lesion is present atthe junction of the OM-2 and posterolateral and extends into the proximal OM-1 and into the continuation of the circumflex. RCA: The RCA is a large dominant ectatic vessel that supplies a moderate-sized PDA (posterior descending artery) and a moderately-sized posterolateral branch. A 90% proximal RCA stenosis is present. A 90% proximal RCA stenosis is present. A 95% stenosis of the proximal PDA is present. A 95% stenosis of the mid-portion of the posterolateral is present."
Naturally, coronary artery bypass was recommended.
Further, my cardiologist said he estimates that my life expectancy decreases by 10 to 12 % each year I do not opt for a CABG. Since I have had CAD for at least four years, that means I have decreased my life expectancy by 40-48% already. He presented this statistic to me, he said, to show me how important it was for me to have a CABG as soon as possible.
Instead, I will continue my medical regimen that was started by Dr. Wayne. I will continue my Metapropolol at 100mg twice a day and Fosinopril 10mg at bedtime. I also asked the cardiologist to writ a prescription for Isodril to be given as follows: 5mg at 7 am, 10 mg at 1 pm and 15 mg at 7 pm. I asked him to write a prescription for moduretic, but he refused, saying a diuretic is not indicated. I will ask my family doctor to write a script for that.
Starting tomorrow, I will record my pulse and blood pressure three times a day and track the times I take my medications and any signs and symptoms present, on a daily basis. I will record that data here, in much the same way I did when I started this blog four years ago. I hope you will follow my progress with me. I ill be happy to entertain any comments and questions and post them all here.
The angiogram report stated :
LAD: "The LAD (left anterior descending) artery is a large vessel in its proximal segment and then tapers in it mid-segment to a long region of diffuse 80-90% disease. A moderate-sized first diagonal is present with an 80% proximal stenosis. The apical LAD is large enough for bypass grafting."
Circumflex: "The circumflex is a moderate-sized vessel that supplies a moderate-sized OM-1, a moderate-sized branching OM-2 and a moderate-sized posterolateral. A 99% subtotal lesion is present in the ostial/proximal OM-1. A subtotal bifurcation lesion is present atthe junction of the OM-2 and posterolateral and extends into the proximal OM-1 and into the continuation of the circumflex."
RCA: The RCA (right coronary artery) is a large dominant ectatic vessel that supplies a moderate-sized PDA (posterior descending artery) and a moderately-sized posterolateral branch. A 90% proximal RCA stenosis is present. A 90% proximal RCA stenosis is present. A 95% stenosis of the proximal PDA is present. A 95% stenosis of the mid-portion of the posterolateral is present."
Hemodynamics: "Hemodynamic assessment demonstrates no systemic hypertension and mildly elevated LVEDP 15 mmHg."
Coronary Circulation: "Left Main:Normal. The LAD (left anterior descending) artery is a large vessel in its proximal segment and then tapers in it mid-segment to a long region of diffuse 80-90% disease. A moderate-sized first diagonal is present with an 80% proximal stenosis. The apicala LAD is large enough for bypass grafting. Circumflex: The circumflex is a moderate-sized vessel that supplies a moderate-sized OM-1, a moderate-sized branching OM-2 and a moderate-sized posterolateral. A 99% subtotal lesion is present in the ostial/proximal OM-1. A subtotal bifurcation lesion is present atthe junction of the OM-2 and posterolateral and extends into the proximal OM-1 and into the continuation of the circumflex. RCA: The RCA is a large dominant ectatic vessel that supplies a moderate-sized PDA (posterior descending artery) and a moderately-sized posterolateral branch. A 90% proximal RCA stenosis is present. A 90% proximal RCA stenosis is present. A 95% stenosis of the proximal PDA is present. A 95% stenosis of the mid-portion of the posterolateral is present."
Naturally, coronary artery bypass was recommended.
Further, my cardiologist said he estimates that my life expectancy decreases by 10 to 12 % each year I do not opt for a CABG. Since I have had CAD for at least four years, that means I have decreased my life expectancy by 40-48% already. He presented this statistic to me, he said, to show me how important it was for me to have a CABG as soon as possible.
Instead, I will continue my medical regimen that was started by Dr. Wayne. I will continue my Metapropolol at 100mg twice a day and Fosinopril 10mg at bedtime. I also asked the cardiologist to writ a prescription for Isodril to be given as follows: 5mg at 7 am, 10 mg at 1 pm and 15 mg at 7 pm. I asked him to write a prescription for moduretic, but he refused, saying a diuretic is not indicated. I will ask my family doctor to write a script for that.
Starting tomorrow, I will record my pulse and blood pressure three times a day and track the times I take my medications and any signs and symptoms present, on a daily basis. I will record that data here, in much the same way I did when I started this blog four years ago. I hope you will follow my progress with me. I ill be happy to entertain any comments and questions and post them all here.
Today is the Day
I do battle with the medical/industrial complex today at 11:30 am. I will be meeting with my cardiologist, who will be making the case for a quintuple coronary artery bypass graft. He will make it sound as if he solely has my best interests in mind. What he will not discuss is the fact that not only does the surgeon and team performing the surgery have a vested interest in promoting CABG surgery as much as possible, so does the hospital in which the procedure will be performed and even my cardiologist, who may be asked to stand by if needed. Even physical therapists will benefit from me undergoing a CABG. About the only person in this whole equation who stands to lose anything if this surgery is performed is me, the patient.
Thus far, since 2004, when a cardiologist and cardio-thoracic surgeon attempted to coerce me into a quintuple CABG I didn't need, I have cost these physicians, ancillary personnel perhaps a quarter of a million dollars in lost revenue derived from the performance of a CABG on my body. Since I am still alive and kicking after I was told I would probably die of a stroke or heart attack in a few weeks or months if I didn't have the surgery, I guess I proved these medicos wrong.
In 2004 and again in 2008, I was told my heart was in great shape. My coronary arteries sucked, but the pump was in fine condition. Obviously the heart is receiving the oxygenated blood these arteries were designed to provide. My body, without the help of a huge surgical team, is creating a collateral vessel system that takes over from the damaged arteries. Common sense tells you, if you do any cutting in that area, you stand to damage the collateral vessel system. When a CABG is performed on a heart that is in great shape, that organ is irrepairably damaged. I don't think that is a good thing.
So today I will meet with my cardiologist whose job it is to coerce and frighten me into a CABG, a procedure I am adamantly opposed to receiving. CAD and its treatment are two things I have studied for four years. I do not go into this battle to maintain control of my medical treatment plan lightly. I understand what's at stake if I am wrong and realize if I am wrong, I may pay the ultimate price. However, I have been right for four years so I've got a pretty good track record.
When I return from my appointment with my cardiologist, I will add another entry to this blog.
Thus far, since 2004, when a cardiologist and cardio-thoracic surgeon attempted to coerce me into a quintuple CABG I didn't need, I have cost these physicians, ancillary personnel perhaps a quarter of a million dollars in lost revenue derived from the performance of a CABG on my body. Since I am still alive and kicking after I was told I would probably die of a stroke or heart attack in a few weeks or months if I didn't have the surgery, I guess I proved these medicos wrong.
In 2004 and again in 2008, I was told my heart was in great shape. My coronary arteries sucked, but the pump was in fine condition. Obviously the heart is receiving the oxygenated blood these arteries were designed to provide. My body, without the help of a huge surgical team, is creating a collateral vessel system that takes over from the damaged arteries. Common sense tells you, if you do any cutting in that area, you stand to damage the collateral vessel system. When a CABG is performed on a heart that is in great shape, that organ is irrepairably damaged. I don't think that is a good thing.
So today I will meet with my cardiologist whose job it is to coerce and frighten me into a CABG, a procedure I am adamantly opposed to receiving. CAD and its treatment are two things I have studied for four years. I do not go into this battle to maintain control of my medical treatment plan lightly. I understand what's at stake if I am wrong and realize if I am wrong, I may pay the ultimate price. However, I have been right for four years so I've got a pretty good track record.
When I return from my appointment with my cardiologist, I will add another entry to this blog.
Friday, February 01, 2008
Inaccurate and Unreliable
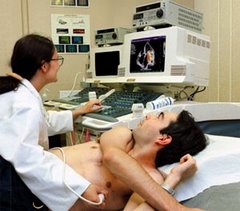
That is what Dr. Howard Wayne called angiograms -- inaccurate and unreliable tests that won't diagnose coronary artery disease. When I arrived at t he Indiana Heart Hospital early in the morning of January 30, I came armed with Dr. Wayne's first book, Living Longer With Heart Disease: The Noninvasive Approach That Will Save Your Life. Published in 1998, this book probably has prevented more patients from undergoing unnecessary coronary artery bypass grafts than any other. It tells it like it is.
Since I owned two copies of this book, I decided to give one to the cardiologist who would be performing my cardiac catheterization, Dr. Michael Robertson. I like Dr. Robertson just as I liked the first cardiologist to urge me to undergo a quintuple CABG four years earlier, Dr. Cory. I like both men. They are friendly and personable, two disarming qualities that may cause prospective patients to let their guards down when told they need a bypass.
I put a bookmark at Chapter 10, the one that discusses the angiogram. I handed the book to Dr. Robertson as I was being wheeled to the cath lab. He graciously took the book and promised to read it, laughing at my audacity of putting the bookmark in the appropriate chapter.
Dr. Wayne said, "The Holy Grail for cardiologists is the angiogram. It is worshipped with a religious fervor unlike any test in medicine. Go to any invasive or interventional cardiologist, and he or she will invariably recommend an angiogram either the same day or the next day -- and will often become upset if you refuse."
He goes on to ask, "Is the cardiologist's faith in this procedure justified? Is the information the angiogram provides reliable? Can it tell the doctor how his or her patient should best be treated, and if they are likely to have a heart attack or die? Will it provide information that can't be obtained in any other way? And, most importantly, is it even necessary to know whether and where an artery is narrowed to treat the patient? In simple terms, is the angiogram recommended for the patient's -- or for the doctor's benefit?
Without going into details, let me tell you how Dr. Wayne answers his own questions in Chapter 10:
"It cannot be emphasized strongly enough that the coronary angiogram is one of the most inaccurate and unreliable tests in all of cardiology. More often than not, it leads to the wrong diagnosis and results in inappropriate and unnecessary treatment. It has little relationship to symptoms, it does not relate to the cause of the patient's symptoms, it correlates poorly with the function of the heart and it cannot accurately predict the occurrence of a heart attack. Immediate angiograms are done solely for economic reasons, not medical reasons."
The chapter concludes with a list of 23 references by cardiologists, scientists and other medical researchers that validate Dr. Wayne's opinion o the coronary angiogram.
Since I owned two copies of this book, I decided to give one to the cardiologist who would be performing my cardiac catheterization, Dr. Michael Robertson. I like Dr. Robertson just as I liked the first cardiologist to urge me to undergo a quintuple CABG four years earlier, Dr. Cory. I like both men. They are friendly and personable, two disarming qualities that may cause prospective patients to let their guards down when told they need a bypass.
I put a bookmark at Chapter 10, the one that discusses the angiogram. I handed the book to Dr. Robertson as I was being wheeled to the cath lab. He graciously took the book and promised to read it, laughing at my audacity of putting the bookmark in the appropriate chapter.
Dr. Wayne said, "The Holy Grail for cardiologists is the angiogram. It is worshipped with a religious fervor unlike any test in medicine. Go to any invasive or interventional cardiologist, and he or she will invariably recommend an angiogram either the same day or the next day -- and will often become upset if you refuse."
He goes on to ask, "Is the cardiologist's faith in this procedure justified? Is the information the angiogram provides reliable? Can it tell the doctor how his or her patient should best be treated, and if they are likely to have a heart attack or die? Will it provide information that can't be obtained in any other way? And, most importantly, is it even necessary to know whether and where an artery is narrowed to treat the patient? In simple terms, is the angiogram recommended for the patient's -- or for the doctor's benefit?
Without going into details, let me tell you how Dr. Wayne answers his own questions in Chapter 10:
- It is impossible to tell if the coronary artery disease seen on an angiogram is old or new in most cases, because there usually are no other angiograms to compare it to.
- There is no correlation between a patient's symptoms and the severity of coronary artery narrowing.
- There are noninvasive tests that are more accurate than the angiogram. The echocardiogram is one of them.
- An angiogram cannot determine the source of a patient's chest pain.
- An angiogram cannot predict a heart attack.
- The findings on an angiogram do not relate to the clinical course of the patient with coronary artery disease.
- Angiograms do not correlate with symptoms, prognosis, cardiac function, and blood flow to the heart muscle.
"It cannot be emphasized strongly enough that the coronary angiogram is one of the most inaccurate and unreliable tests in all of cardiology. More often than not, it leads to the wrong diagnosis and results in inappropriate and unnecessary treatment. It has little relationship to symptoms, it does not relate to the cause of the patient's symptoms, it correlates poorly with the function of the heart and it cannot accurately predict the occurrence of a heart attack. Immediate angiograms are done solely for economic reasons, not medical reasons."
The chapter concludes with a list of 23 references by cardiologists, scientists and other medical researchers that validate Dr. Wayne's opinion o the coronary angiogram.
Subscribe to:
Posts (Atom)