High death rate found in one class of operations at Altoona during 2005
A state group that tracks health care performance found a high death rate for Altoona Regional Health System and one of its surgeons for one type of heart operation in 2005.
The Pennsylvania Health Care Cost Containment Council found the higher-than-expected death rate for heart valve operations in patients who died at the hospital or within 30 days of their procedures.
The high death rate finding for the hospital was based on 59 valve operations.
The same finding for Dr. John Anastasi was based on the 50 valve operations he performed.
The hospital spoke of extenuating circumstances in a letter about the findings to the agency.
“The patients that did not fare well in the current reporting period had many complicating factors, including very advanced age, end-stage heart disease, whose only remaining option was surgery, and emergency cases performed during an acute life-threatening event,” wrote David Cowger, senior vice president of quality/medical affairs. “Many of these patients had pre-existing multi-organ disease compounding their acute cardiac care. Patient and family directives frequently limited the amount of support we could provide.”
To calculate red-flag rates, the agency uses a formula that takes into account how sick patients are.
The council also found higher-than-expected readmission rates within seven days and 30 days for the valve operations at the hospital and for those done by Anastasi.
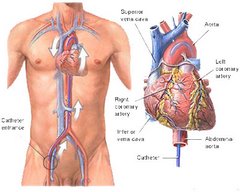
And it found a higher-than- expected readmission rate within 30 days for the 89 coronary artery bypass graft surgeries performed by Anastasi.
The council, a quasi-governmental agency, tracks and reports performance by hospitals and in some cases individual doctors because “there is evidence that information contained in reports such as this encourages hospitals and surgeons to examine their processes and make changes that can improve quality of care and ultimately save lives,” the agency stated in its report.
Altoona constantly monitors its care to improve outcomes, Cowger wrote. All cases of “less-than-optimal outcome are reviewed,” he wrote.
The open-heart surgery team at the hospital has not had significant changes since it began in 1989, he wrote.
The 2005 report also lists Dr. Burt Fazi as performing heart surgery.
Statewide, the council found the in-hospital death rate for coronary bypass surgery patients declined in 2005, while the rates of readmission increased slightly during the same period.
The 2005 mortality rate among bypass patients was 1.9 percent, down from nearly 2 percent the previous year and from 2.4 percent in 2000.
At the same time, 5.5 percent of bypass patients were readmitted within seven days of being discharged — up from 5.2 percent — and 13.6 percent were readmitted within 30 days of being discharged, up from 13.2 percent.
Heart failure, infections and abnormal heart rhythms were the top three reasons for readmissions.
The council has published annual reports on bypass surgeries and how much hospitals charge for them since 1992. This year, it added information on heart-valve procedures, which are more invasive and complicated than bypasses, and included payment data on both procedures for the first time.
‘‘The provider community has argued for a long time that [hospital] charges do not reflect what is paid,’’ said Marc P. Volavka, the council’s executive director. ‘‘The public now has available precisely the kind of information they’re going to need.’’
UPMC was paid thousands more for cardiac surgery
But study says care, measured by deaths and readmissions, was not superior to lower-cost hospitals
A ground-breaking report released today reveals wide disparities in the amounts Pittsburgh-area hospitals received for cardiac surgeries, with the University of Pittsburgh Medical Center paid thousands more than its rivals without offering a superior level of care as measured by mortality and readmission rates.The variations are no surprise to insurers, who provided 2005 payment data for the report, produced by the Pennsylvania Health Care Cost Containment Council. And consumers are unlikely to change hospitals based on the pricing information because health plans shoulder the bulk of the cost of their care.
But one small business representative hopes the new data will motivate employers to demand a greater equality in pricing from hospital to hospital.
"If you are going to charge more, you have to show a better result," said Cliff Shannon, who represents small- and medium-sized manufacturers as president of SMC Business Councils in Churchill. "That is what we expect when we buy a car. God knows, health care is more important than the car we drive."
Referring to UPMC, the nonprofit hospital conglomerate that has major operations in Oakland, he asked: "What kind of rational decision is it to go into the city, find parking in Oakland and have the surgery cost 50 percent more? For a lot of employers, those are the questions that will echo in their heads as they think about their next health care budget."
The two highest-paid hospitals, according to the state agency that seeks to address the cost and quality of health care, were UPMC Presbyterian and UPMC Shadyside, two of 19 institutions controlled by the region's dominant medical provider and biggest employer. Together, in 2005, the East End hospitals received an average of $34,803 for coronary artery bypass graft surgery -- used on patients with significant artery blockage.
No hospital in the area received more. The average payment for the same procedure at the North Side's Allegheny General Hospital was $23,715, while at Jefferson Regional Medical Center in the South Hills, the cost was even lower: $18,009.
Yet the level of care at Jefferson Regional and Allegheny General, as measured by mortality and re-admission rates, was not inferior to that at the two UPMC facilities. In fact, Allegheny General had a lower readmission rate than its crosstown rival.
"There are dramatic differences in payment within the region that don't make a lot of sense," said Marc Volavka, executive director of the cost containment council. "Someone has to ask, 'Why'?"
The statewide report "shows that quality of care has no apparent relationship to the cost of care," said Mr. Shannon, also a board member of the cost containment council. "More expensive does not equal better; less expensive does not equal worse. How much of a premium should we have to pay to go to the brand-name hospitals in Pittsburgh when the quality of care is no better?"
The release of this report, more than a year in the making, provides greater transparency to the often-opaque discussion of rising health care costs across the region and the state
The report is unusual for including average payments made to hospitals for patients covered by commercial insurance. Past reports typically included "charges" -- the amount a hospital bills for a patient's care -- but not the final payment. Hospitals generally do not receive full reimbursement for their charges because insurers or other large purchasers negotiate discounts.
While the two UPMC hospitals had the highest commercial payment rate in the region for coronary artery bypass surgery, some hospitals elsewhere in the state were paid more.
Philadelphia's Hahnemann University, for example, had an average payment of $78,312. At the Hospital of the University of Pennsylvania, the figure was $60,733. Temple, also in Philadelphia, was paid $57,533 for the same procedure.
UPMC spokesman Wendy Zellner cited those differences as a better point of comparison, since they are all academic medical centers, like UPMC, and in that group, UPMC Presbyterian and Shadyside have the highest volume of bypass surgeries and the lowest average payment rates.
Within southwestern Pennsylvania, "various factors affect average charges and payment, including the nature and complexity of the cases that we treat," Ms. Zellner said. The growth in patient volume at UPMC "suggests that insurers and patients believe that we are providing high quality care at a fair price."
Higher prices for UPMC services were an issue last month when the state attorney general's office announced an agreement regarding the planned merger of the region's largest health system with Mercy Hospital.
State officials didn't want the merger to result in higher prices at Mercy, noting that they are currently lower than at UPMC. Health system officials agreed to extend existing health plan contracts at Mercy and their pricing for eight years, with allowances for inflation. Before it could take place, the merger also would need approval from the Federal Trade Commission and the Vatican.
At Mercy, the average payment for a coronary artery bypass was $25,315 -- almost $10,000 less than at the two UPMC facilities (but more than the $24,834 paid to UPMC Passavant, a community hospital in the North Hills). "I don't know if I can explain that great discrepancy," said Dr. Ross DiMarco Jr., chief of cardiovascular and thoracic surgery at Mercy.
West Penn Allegheny Health System, parent of the West Penn Hospital and Allegheny General, raised the same question yesterday, noting that its hospitals performed "on par or better" than the two UPMC hospitals in the East End and still UPMC is paid more.
"In any other market, quality and efficiency are rewarded," said Tom Chakurda, spokesman for West Penn Allegheny. "That does not appear to be the case in health care."
Despite the variation in payment, mortality and hospital readmission rates at local hospitals were generally what would be expected for bypass and valve surgeries, according to the cost containment council report. Some facilities, including Allegheny General, St. Clair Memorial and The Medical Center, Beaver, had lower-than-expected rates for some surgeries. Washington and Westmoreland Regional hospitals, however, had some that were higher than expected.
For a variety of reasons, large medical centers are able to negotiate higher payment rates from insurers or other purchasers, said Dr. Carey Vinson, vice president for quality and medical performance management at Highmark.
The medical care they provide, along with teaching and research, represent "a unique set of services to the community," Dr. Vinson said. "They parlay that into asking for greater reimbursement."
Large centers also contend they treat more complex needs and have higher costs, he said.
But smaller hospitals also try to strengthen their negotiating position -- for example, by noting if they are the only medical facility in a particular area, Dr. Vinson said.
"All hospitals try to leverage their uniqueness when they can," he said.
Medicare payment rates for the cardiac surgeries also varied, according to the report. Medicare officials noted that those rates can be affected by a number of factors, including whether hospitals are teaching facilities or serve large numbers of poor patients.
The report also noted that mortality rates, lengths of stay and payments were much higher when patients having the cardiac surgeries acquired infections in the hospital.
Jessica Seabury, executive director of the Consumer Health Coalition, said payment incentives are needed that better promote good care. Her group works to increase access to quality, affordable health care in southwestern Pennsylvania.
Carolyn Scanlan, president of the Hospital & Healthsystem Association of Pennsylvania, the hospital industry's main lobby in the state, noted that the report indicates that in-hospital mortality rates for cardiac bypass surgeries have continued to drop. She said more study is needed concerning the payment data and information on hospital-acquired infections and lengths of stay.