The study used recent data to confirm and update knowledge of racial disparities persisting in the health care system.
"We found some significant differences, and definitely, we have no good explanation for why," said lead researcher Dr. Ioana Popescu, health services researcher at Iowa City VA Medical Center. "More research needs to be done."
The study is published in the June 13 issue of the Journal of the American Medical Association.
"This study uses a contemporary cohort, following patients through 2005, and this is the first study to look at that," said Popescu, who is also a junior faculty member at the University of Iowa Carver College of Medicine in Iowa City.
The study also differs from previous research in that it stratifies patients by hospital type, meaning those that do and do not provide specialized heart services.
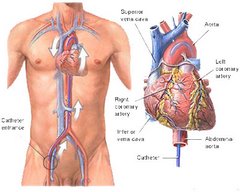
Prior studies have indicated that racial differences in care after a heart attack appear most pronounced when it comes to invasive and costly technologies such as coronary revascularization or procedures to get the blood flowing again to the heart.
The most common type of revascularization is coronary artery bypass graft (CABG).
Some recent studies have suggested that differing access to high-quality providers might account for some racial disparities.
Less than one-fifth of U.S. acute-care hospitals provide coronary revascularization, and many Medicare beneficiaries are initially admitted to hospitals that don't provide CABG or percutaneous coronary intervention (PCI, formerly known as angioplasty).
Few studies have looked at such patterns of care and how they might impact disparities.
For this study, the authors looked at more than 1.2 million black and white Medicare beneficiaries aged 68 and older who had been admitted to one of 4,627 U.S. hospitals between 2000 and 2005 with a heart attack. The hospitals were mixed, some having revascularization services and some not.
Black patients admitted to hospitals with or without revascularization services were less likely to undergo revascularization than white patients (34.3 percent vs. 50.2 percent and 18.3 percent vs. 25.9 percent) and were also more likely to die within one year (35.3 percent vs. 30.2 percent and 39.7 percent vs. 37.6 percent).
In addition, black patients admitted to hospitals without these specialized services were less likely to be transferred to a hospital with the services within two days (7.4 percent versus 11.5 percent) and within 30 days (25.2 percent versus 31 percent) of admission.
The likelihood that a black patient admitted to a hospital without revascularization services would be transferred was also 22 percent lower than their white counterparts, the team found.
Even among patients who were transferred, blacks were 23 percent less likely to undergo revascularization.
Blacks had a 9 percent lower risk of death during the first 30 days after admission to the hospitals with revascularization services and 10 percent lower in the other hospitals. Between 30 days and one year after admission, blacks had a 12 percent to 26 percent higher risk of death. The risks were lower if the patient underwent revascularization but were still higher than for whites.
Some aspects of the data were unclear, however, including what type of heart attack the participants suffered. The guidelines for revascularization can be different depending on the characteristics of the heart attack, noted Dr. John P. Erwin III, associate professor of internal medicine at Texas A&M Health Science Center College of Medicine and cardiologist at Scott & White Hospital in Temple.
It's also unclear why such disparities exist.
"Probably we should look at other potential contributors to the differences that we notice such as more clinical information on patients," Popescu said. "There may be some underlying baseline differences such as symptoms in the beginning, the time they chose to come to the hospital, which may play role in getting the procedure and the diagnosis. Definitely we need more research into patient preferences and decision-making."
"Aspects of medical decision-making were unclear," Erwin added. "More data points would have helped us understand it."
For Dr. John Underwood, a cardiologist in Scottsdale, Ariz., and past president of the Association of Black Cardiologists, the findings confirm previous patterns seen in medicine. And if patients aren't undergoing procedures such as revascularization, then they're less likely to be followed up.
"You're not tied into the system, those things aren't happening, and people are dying," he said.











No comments:
Post a Comment