LATEST MORBIDITY
AND
MORTALITY STATISTICS
ON BYPASS SURGERY
AND
ANGIOPLASTY
Excerpts from Living Longer With Heart Disease:
The Noninvasive Approach That Will Save Your Life
With the exception of the first report in the next paragraph, the following series of reports are presented in chronological order. A common method of describing results is either mortality or freedom from a cardiovascular event such as death, heart attack, stroke or repeat bypass surgery or angioplasty. Mortality figures are presented in a variety of formats such as 3, 5, and 10 year mortality, and so are cardiovascular events. I have modified these figures so that they are on a yearly basis to make comparison easier. The first report (reference 17) is presented out of order because it not only shows the most recent statistics, but it also reflects outcomes in one of the largest group of patients to date.
From a multicenter study (17) from several major medical centers, using New York State's registry for patients undergoing coronary artery bypass surgery or coronary angioplasty, the mortality rate was tabulated for each procedure. I have listed separately the mortality rate on an annual basis for patients with disease involving two coronary arteries, and for patients with disease of all three coronary arteries. Keep in mind that the annual mortality for patients with two and three vessel disease who are treated conservatively with appropriate medication is less than 1% per year.
In 17, 857 patients with disease of all three coronary arteries who underwent coronary artery bypass surgery, the annual mortality rate was 3.3 %. In 1,294 patients with three vessel disease who underwent coronary angioplasty the annual mortality rate was 4.2 %.
In 9,212 patients with two vessel disease undergoing coronary artery bypass surgery, the annual mortality rate was 2.7 %. In 7,405 patients with two vessel disease undergoing coronary angioplasty the annual mortality rate was 2.3 %.
For mortality related to age, see the National Medicare Experience below.
Dr. Salem Yusuf reviewed the medical literature from 1972 to 1984 and compared the mortality of medical and surgical treatment. (18) There were four studies involving a total of 416 patients. At 10 years the mortality of the surgically treated patients was 33% or 3.3% per year. The mortality of the medically treated patients at 10 years was 34% or 3.4% per year. It is to be noted that this reflects the medical treatment primarily of the Seventies.
Dr. Spencer King of Emory University compared 194 bypass surgery patients with 198 angioplasty patients. The annual mortality for the bypass surgery patients was 2.1% per year and that for the angioplasty patients 2.4% per year. (19)
In a study of mortality rates in different age groups in Medicare patients undergoing either bypass surgery or angioplasty, Dr. Eric Peterson and his associates at Duke University Medical Center found the following. (20)
THE NATIONAL MEDICARE EXPERIENCE
|
| Mortality After Angioplasty
225,915 patients |
| Mortality After Bypass Surgery
357,885 patients |
| Ages | 30 Day | 1 Year | | 30 Day | 1 Year |
|
| % | % |
| % | % |
|
|
| 65-69 | 2.1 | 5.2 |
| 4.3 | 8.0 |
| 70-74 | 3.0 | 7.3 |
| 5.7 | 10.9 |
| 75-79 | 4.6 | 10.9 |
| 7.4 | 14.2 |
| >80 | 7.8 | 17.3 |
| 10.6 | 19.5 |
Obviously, mortality rate is related to age. Unfortunately, rarely are these figures quoted to elderly patients when they are urged to undergo these procedures.
In a study of 591 patients from nine medical centers in North America, the in-hospital complication rate was Death 1.5%, Heart Attack 4.2%, Emergency Bypass 3.2% and Total Complications 15.4%. (21) This does not include complication rates after discharge from the hospital.
From the University of Washington in Seattle comes a study of the 15 year survival rate of the Coronary Artery Surgery Study of 6,018 men and 1,095 women who originally underwent treatment between 1974 and 1979. For medical treatment the 15 year survival rate for men was 50% and 49% for women. For those with initial surgical treatment the survival for men was 52% and 48% for women. Thus, there was no significant difference in survival between the two treatments with the annual mortality being 3.3%.
Another interesting study was the CAVEAT Trial (Coronary Angioplasty Versus Excisional Atherectomy Trial).(23) Atherectomy refers to the use of a rotor rooter type of device that is inserted into a coronary artery and the arteriosclerotic plaque is cut up and scooped out. In this study only the frequency of a myocardial infarction (heart attack) was studied in 500 patients undergoing angioplasty and 512 having atherectomy. The incidence of myocardial infarction in the atherectomy patients was 15.2% and it was 6.8 % in the angioplasty patients. The high incidence of heart attacks with both groups was because cardiac enzymes were measured rather than merely getting an electrocardiogram after the procedure. Thus, the reported incidence of myocardial infarction after these procedures is artificially low because insensitive methods of detection are being used.
Another report dealing with mortality rate in elderly patients undergoing cardiac surgery is from Cedars-Sinai Medical Center in Los Angeles. (24) In a study of 528 patients over 80, the 30 day mortality was 8.3%. At one year it was 18% and at 5 years 38%. These figures are very similar to the Duke study.
From the St. Louis University Health Sciences Center (25) a review of 250 patients undergoing coronary artery bypass surgery found that the annual mortality for patients between 60 and 79 was about 7% per year and for patients above the age of 80 it was 13% per year.
From the National Registry of Myocardial Infarction in 3,648 patients undergoing angioplasty who had this procedure done initially as the primary treatment, the in-hospital mortality for patients who were treated under one hour was 6.9%, from 1-2 hours 5.7%, from 2-3 hours 9.1%, and after three hours 9.4%. (26) These are not small numbers. In my experience the mortality rate of a heart attack patient after he or she reaches the hospital is excellent. There is a better than 95% chance of recovery, even better if the patient gets to the hospital early. Thus, the mortality rate for patients treated with angioplasty in this study is twice as great as with conservative medical treatment. A recent Veterans Administration Study showed similar findings in a group of 500 patients with an acute heart attack. There were 21 patients who died in the surgery or angioplasty treated group at nine days, but only six patients who died in the medically treated group in this time period.
Looking at mortality figures alone doesn't tell the complete story. Perhaps a better way to evaluate the outcome of these procedures is to combine all cardiovascular events including death on an annual basis. It is known, for example, the after angioplasty, the coronary artery that was dilated will usually become narrowed again and may close off. The frequency with which this happens is about 50%. How often this will result in repeat symptoms is not precisely known. The following reports describes recurrences of cardiovascular events including death, heart attack, unstable angina, repeat angioplasty and coronary artery bypass surgery.
From the Massachusetts General Hospital in a trial of 127 patients undergoing angioplasty or coronary artery bypass surgery, the annual cardiovascular event rate was 7.7% per year for the surgery patients and 17.7% per year for angioplasty patients. (27)
From the Thorax Center at Erasmus University in Rotterdam, a 10 year study of 856 patients undergoing angioplasty revealed an annual mortality rate of 2.2% and an annual cardiovascular event rate of 8.6%. (28)
In the BARI trial (Bypass Angioplasty Revascularization Investigation), 1,829 patients were followed for 5.4 years. (29) Annual mortality was 2.1% per year for bypass surgery and 2.7% per year for angioplasty. Event rate was 4% per year for surgery and 4.3% per year for angioplasty.
In a 10 year study from St. Antonius Hospital in the Netherlands, 351 patients who had angioplasty were followed.(30) Annual mortality was 2% per year and cardiovascular event rate 10% per year.
From the University of North Carolina at Greensboro, 633 patients who were treated with primary angioplasty for their heart attack were followed for 5.3 years. The in-hospital mortality was very high at 9% and the cardiac mortality at five years was another 9%.(31) Total mortality was twice what it should have been.
From the University of Ottawa Heart Institute in Ontario, Canada, a 25 year study of 1,388 patients who underwent bypass surgery at an average age of only 48 years reveals an annual mortality of 2%. Eighteen percent had to undergo repeat surgery during this period. (32)
From the Veterans Affairs Medical Center and the University of Colorado Health Sciences Center in Denver comes a study of 131 patients above the age of 70 with unstable angina who underwent coronary angioplasty for their symptoms. The mortality at 30 days was a striking 13%. (33)
In a comparison of medical treatment versus angioplasty for patients with stable coronary artery disease, 20 centers from the United Kingdom and Ireland treated 1,018 patients. The risk of death or a heart attack was 2.3% per year for angioplasty treated patients but only 1.2% per year for medically treated patients. (34)
In a recent Veterans Administration study known as the VANQWISH trial 920 patients from 15 medical centers with an acute heart attack were randomized to treatment with revascularization (angioplasty or coronary artery bypass surgery) or conservative medical treatment. At the time of discharge from the hospital, 21 patients who had undergone revascularization had died versus only six medically treated patients. At 2.5 years there were 80 deaths in the aggressively treated group versus only 59 deaths in the conservatively treated patients.
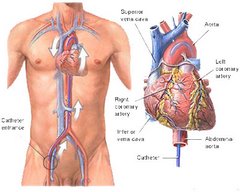
There are only a few reports dealing with the use of stents placed within a coronary artery. A stent is a metal tube that can be expanded when placed within a coronary artery. When fully expanded it becomes a scaffolding that helps to keep the artery from closing. Typically, when an artery is dilated with balloon angioplasty, a delayed complication is collapse of the walls of the blood vessel causing the artery to become blocked. Stents were developed to prevent this from happening. This it does, however, although the vessel walls stay apart, the inside of the stent becomes filled with tissue that grows into the stent. Thus, stents often become occluded and the vessel still closes off.
From Harvard University comes a report on 175 patients who had stents inserted. Annual mortality was 2.7% and annual cardiovascular event rate was 10%. (35)
From the Cardiovascular Division of the University of Pennsylvania the three year outcome of 65 patient who underwent stenting was studied. Mortality was 4% per year and cardiovascular event rate was 14.7% per year. (36)
From the University of Giessen in Germany comes a detailed analysis of 300 patients who underwent primary angioplasty for an acute myocardial infarction.(37) Their findings are described in the following table.
|
| 1 Month | 6 Months | 1 Year | 2 Years | 3 Years |
| All Cardiac Events | 13% | 22% | 34% | 42% | 51% |
| Cardiac Mortality | 4% | 5% | 6% | 7% | 9% |
| Total Mortality | 5% | 6% | 9% | 10% | 13% |
| Repeat Angioplasty |
| 20% | 23% | 25% | 31% |




















Comment from Nancy Reyes
Time: December 5, 2006, 8:10 pm
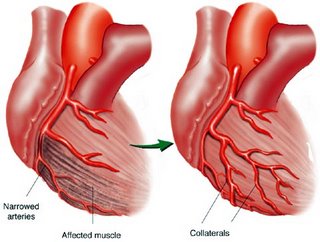
SHHH…we docs know about angiogenesis. And if we could be sure that it would happen in our patients, we could spare the bypass surgery.
You see, I’ve been in medicine before they did bypasses, and you know what? Some people with stable angina lived for years, although many were misearable. Some got better. The only “treatment” was diet and exercize and nitroglycerin back then.
Similarly, we knew that a vegetarian low cal diet combined with a gradual increased exercize program would result in improvement almost as much as surgery. We’ve known that since 1970 (maybe before, but I graduated 1971).
Alas, it doesn’t work in the real world. You try telling grandma she needs to stop eating cannoli.
When they did a comparison study of diet/exercize/medicine vs bypass in the VA, they found the first group ended up having more heart attacks or having so many symptoms the guys insisted on the bypass.
You see, in the real world our patients don’t eat correctly, don’t exercize, and want a quick fix.
Now we have a third choice, stents, but they work better for one or two blockages, not someone with arteries that are full of junk.(i.e. diffuse arteriosclerotic placques).
Now, if these new stem cell injections work, maybe we can stop doing bypasses. Then I’ll agree with you.
In the meanwhile, continue what you’re doing. I love it when patients actually take care of their own health.