Thursday, January 31, 2008
Same Song, Different Verse
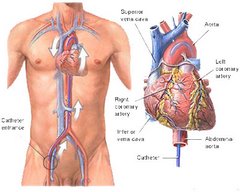
So, I wasn't the least bit surprised when the cardiologist who performed my most recent cardiac catheterization concluded that the angiogram showed I needed a CABG. I would have been more shocked if he suggested the medical treatment I had been undergoing since the spring of 2004 and the Enhanced External Compression Pulsation (EECP) Therapy I took last fall had actually made the most popular cardiac surgery performed in the USA unnecessary, or at the very least, premature.
The first angiogram, performed in 2004, showed I had a 100 percent blockage in two arteries and 85 percent occlusions in three more. The cardiologist who performed that procedure four years ago, adamantly insisted a stroke or heart attack was imminent unless I had an immediate Quintuple CABG performed. He seemed personally insulted by my declaration that I was going to seek a second opinion, making the rash statement, "You are a time bomb waiting to explode." But that obvious attempt to coerce me into consenting to have my chest cracked open didn't work. I stubbornly (some would say stupidly) obtained a second opinion and even had the gall to take the medical advice of the cardiologist who provided that second opinion by choosing his more prudent medication regimen.
Today I underwent a second angiogram. I had hoped it would definitively demonstrate that my decision to opt for a nonsurgical alternative to a CABG was the correct one. It did not. However, the cardiologist at the Indiana Heart Hospital who performed the cardiac catheterization today did say some thing very similar to the doctor who performed the one four years ago. He said, "Your pump is in great shape."
That declaration alone was enough to tell me I chose the proper course in 2004. The cardiologist today said something else that was very telling. He said, "There is at least a trickle of blood going through each of your arteries." Now he said this in response to my question as to why the heart in such great shape if the arteries that feed it oxygen suck. He could have said, "The collateral vessels must be supplying the heart with oxygen." He did not. He specifically attributed the pump's great shape to the small amount of blood still being pumped through my arteries.
The cardiologist today also gave me some good news. He said the angiogram showed the left ventricular artery was not comprimised. That vessel, morbidly known as the "widow-maker" is the one artery that its occlusiion would warrant an immediate CABG.
I have an appointment to see my cardiologist on Monday, next. At that time, I plan on looking at the results of both angiograms I have undergone and the echocardiogram that was performed on Monday. Unless he provides me with a very compelling reason to undergo a CABG, I will continue the treatment of my coronary artery disease as I feel Dr. Howard Wayne would have.
I will report back to the readers of this blog on Monday February 4. In the meantime, I am soliciting the opinions and advice of all who read this blog. What do you think I should do? If it was your decision to make, how would you go about making it? Please provide your comments as soon as possible. See you next week.
Tuesday, January 29, 2008
Angina Attack
By 10 PM, I began experiencing tremors far more severe than any my Parkinson's disease ever caused. I also developed a fairly significant chest pain that lasted a couple of hours and was accompanied by sweating, nausea and vomiting -- classic signs of a myocardial infarction. I stubbornly refused to go to the emergency room and by 2 AM, the symptoms had all subsided and I felt well enough to perform the activity the pills were designed to facilitate. The chest pain returned during this time.
I decided to go to the emergency room and I drove myself to the Indiana Heart Hospital. The emergency room staff swung into action the minute I arrived and emergency treatment was quickly initiated. The monitor was hooked up, an IV established, lab work drawn, oxygen provided by nasal cannula. The on call cardiologist arrived soon after this was done and he intervieiwed and examined me. It wasn't very much longer that a doctor from my own cardiologist's group arrived and I was admitted to an observation unit.
This was the first instance of angina that I experienced since completing EECP last fall. In fact, I had not used nitroglycerin and weaned myself off of Imdur specifically so I would be able to use medications like Viagra, Cialis and Levetra. I had Levetra with me, but foolishly used the natural supplement because it had giveen such excellent results a fortnight before.
Well the good news was, I had not had a heart attack. The markers were all negative and an echocardiogram apparently turned out normal. At least I was allowed to leave the hospital a little more than 12 hours after arriving. But I left with the promise to return Thursday for an angiogram. Now, readers of this blog know I am generally opposed to this invasive test and my favorite noninvasive cardiologist is no doubt spinning in his grave because I signed a consent to undergo this cardiac catheterization. But I was faced with three choices.
One, I could continue taking the prescribed medication that has served to keep me from the cardio-thoracic surgeon's blade for nearly four years and not have the angiogram. This choice is the one I wanted to take at first because Dr. Howard Wayne had little faith in this procedure.
Two, I could have the angiogram with the plan of having stents placed or angioplasty performed. Since I am adamantly opposed to stents, this choice was eliminated as the doctor presented it to me.
Three, I could have the angiogram with the plan to have a CABG done after the procedure is completed. I again said this wasn't a choice, with the caveat that if there was evidence thaat the left ventricular artery was partially occluded, I would consent to the surgery. The "Widow Maker" is a vessel not to be played with.
I did agree to undergoing cardiac catheterization day after tomorrow for one reason. I want to compare the angiogram that was performed in 2004 with this new one. It should tell me if Dr. Wayne's medical regimen and the EECP successfully allowed my body's collateral vessel system to develop around the blocked arteries. So in actuality, I am allowing this invasive procedure to be performed so the efficacy of my treatment thus far can be evaluated.
If my body did create a viable collateral vessel system that effectively supplies my heart with oxygen, I feel that will lend credence to my decision to refuse to have a quintuple bypass four years ago. I am scheduled for the cardiac catheterization on Thursday morning. As soon as I come home from it, I will report the findings on thsi blog.
Sunday, January 27, 2008
Cholesterol Scare
There are many sites on the Internet that say the same thing. There are links to some of these sites right on the webpage you are currently reading. Finally, some mainstream cardiologists agree with the necessity of lowering cholesterol levels. An Op Ed piece in today's New York Times seems to agree with Dr. Wayne.
Here is a portion of the article:
The truth is, we’ve always had reason to question the idea that cholesterol is an agent of disease. Indeed, what the Framingham researchers meant in 1977 when they described LDL cholesterol as a “marginal risk factor” is that a large proportion of people who suffer heart attacks have relatively low LDL cholesterol.
So how did we come to believe strongly that LDL cholesterol is so bad for us? It was partly due to the observation that eating saturated fat raises LDL cholesterol, and we’ve assumed that saturated fat is bad for us. This logic is circular, though: saturated fat is bad because it raises LDL cholesterol, and LDL cholesterol is bad because it is the thing that saturated fat raises. In clinical trials, researchers have been unable to generate compelling evidence that saturated fat in the diet causes heart disease.
The other important piece of evidence for the cholesterol hypothesis is that statin drugs like Zocor and Lipitor lower LDL cholesterol and also prevent heart attacks. The higher the potency of statins, the greater the cholesterol lowering and the fewer the heart attacks. This is perceived as implying cause and effect: statins reduce LDL cholesterol and prevent heart disease, so reducing LDL cholesterol prevents heart disease. This belief is held with such conviction that the Food and Drug Administration now approves drugs to prevent heart disease, as it did with Zetia, solely on the evidence that they lower LDL cholesterol.
But the logic is specious because most drugs have multiple actions. It’s like insisting that aspirin prevents heart disease by getting rid of headaches.
One obvious way to test the LDL cholesterol hypothesis is to find therapies that lower it by different means and see if they, too, prevent heart attacks. This is essentially what the Vytorin trial did and why its results argue against the hypothesis.
Other such tests have likewise failed to confirm it. A recent trial of torcetrapib, a drug that both raises HDL and lowers LDL cholesterol, was halted midstream because the drug seemed to cause heart attacks and strokes rather than prevent them. Estrogen replacement therapy also lowers LDL cholesterol, but it too has failed to prevent heart disease in clinical trials. The same goes for eating less saturated fat.
So it is reasonable, after the Vytorin trial, to question the role of LDL cholesterol in heart disease. Not whether statins help prevent heart disease, but whether they work exclusively, or at all, by this mechanism.
There are numerous other ways in which statins might be effective. They reduce inflammation, which is now considered a risk factor for heart disease. They act to keep artery walls healthy. And statins act on lipoproteins as much as on the cholesterol inside them. They decrease the total number of low-density and very low-density lipoproteins in the blood, including the smallest and densest form of LDL, which is now widely believed to be particularly noxious.
Because medical authorities have always approached the cholesterol hypothesis as a public health issue, rather than as a scientific one, we’re repeatedly reminded that it shouldn’t be questioned. Heart attacks kill hundreds of thousands of Americans every year, statin therapy can save lives, and skepticism might be perceived as a reason to delay action. So let’s just trust our assumptions, get people to change their diets and put high-risk people on statins and other cholesterol-lowering drugs.
Science, however, suggests a different approach: test the hypothesis rigorously and see if it survives. If the evidence continues to challenge the role of cholesterol, then rethink it, without preconceptions, and consider what these other pathways in cardiovascular disease are implying about cause and prevention. A different hypothesis may turn out to fit the facts better, and one day help prevent considerably more deaths.
I trusted Dr. Wayne implicitly with my medical treatment. He was my second opinion after I was told in the spring of 2004 that I was a walking time bomb and if I didn't have an immediate quintuple bypass, I would probably have a stroke or heart attack within a few months. If medical terrorists are trying to coerce you into having a surgical procedure, especially the big money maker, Coronary Artery Graft Bypass, run, don't walk, to the nearest noninvasive cardiologist for a second opinion.
Monday, January 21, 2008
Still Angina-Pain-Free
Since I had no angina pain, I had not used nitroglycerin in about three months. I was still taking 30mg of Imdur twice a day. Since I was between cardiologists, I asked my family physician how I should go about weaning myself off the Imdur. We decided I should take 15mg three times a day for a week to 10 days then decrease to 15mg twice a day for a week to 10 days, and finally take 15mg once a day for a week to 10 days. If I were to experience angina during the time I was titrating down the Imdur, I was to increase the dose to the previous level and see my doctor.
Fortunately the weaning went without any untoward effects. My blood pressure now is running about 120/70. Since I got off of the Imdur, I saw a new cardiologist. He gave me a physical and declared me to be in good enough shape that I don't have to see him for a year. He also prescribed Levitra for erectile dysfunction. I am potent again!
I started physical therapy last month for a balance and gait problem I have that is related to my Parkinson's disease. I have been going twice a week for a month now. The therapist has me warm up on a stationary bike or stair step machine before she puts me through my paces. I am getting an excellent workout and still am angina-pain-free.
Those of you who have been reading this blog know that way back in the spring of 2004, I was strongly coerced by a cardiologist to get a quintuple coronary artery bypass graft. I chose to get a second opinion from a noninvasive cardiologist who started me on medication. I did quite well on the medical regimen until the fall of 2006 when the angina pain returned. My new cardiologist was willing to allow me to manage my own medical treatment plan but he strongly suggested I have the bypass. I asked him what he thought about EECP and he said it may be a good choice for someone who is not a candidate for the bypass or who, for other reasons, refused to have the surgery.
The EECP worked extremely well and this April I will celebrate four years since being told I was a walking time bomb who could have a stroke or heart attack at any time. So, once again, I recommend that anyone who is told he needs a bypass get a second opinion. And don't get that second opinion from any old cardiologist. Go to a NONINVASIVE cardiologist.
Tuesday, January 01, 2008
Happy New Year
I don't remember the last time I put a nitroglycerin tablet under my tongue. I have gone from taking 30 mg of Imdur twice daily to taking 15 mg a day now. Next week I will be seeing a new cardiologist and hope he completely weans me off of the Imdur. Of course, those of us who must take nitro and Imdur realize you cannot take drugs that treat erectile dysfunction when you are on them.
In my mind, I have proven that EECP is an excellent and more than adequate substitute for coronary artery bypass graft (CABG). I hope anyone being coerced by their cardiologists to get a bypass will do what i did in 2004 -- get a second opinion from a noninvasive/noninterventional cardiologist. By doing so, I have dodged the cardio-thoracic surgeons sharp scapel four nearly four years
Sunday, October 28, 2007
Still Ticking
My stamina and physical endurance are better that than they were pre-EECP therapy. I sleep better at night and have not taken naps in the day. My mobility is better. I get out of bed with much less struggling than before and most of problems I do have moving I attribute to my Parkinson's disease.
I would recommend EECP to anyone who has coronary artery disease and who do not want to undergo the traumatic and invasive surgical coronary artery bypass graft. Three years and seven months ago, I was told by a cardiologist that I was a walking time bomb. He wanted me to undergo a quintuple bypass two days later. I decided to get a second opinion and am certainly glad I did.
If anyone wants to ask questions about my EECP experience or any other aspect of my experience with angina and coronary artery disease, please leave a comment.
Tuesday, October 02, 2007
The Countdown Begins

Well, just ten more therapy sessions and I'll be done with my EECP. While the results are not yet what I had hoped them to be, the angina has decreased in frequency, length and intensity. I haven't used nitroglycerin in at least a week. My stamina is generally better although I do take a short nap most days and I didn't before beginning EECP.
I had hoped I might have a complete absence of angina symptoms as I did for over two years on Dr. Wayne's medication regimen. I would definitely say so far EECP has been a success so far.
Friday, September 21, 2007
A Junkie's Brain & Parkinson's
From Wired.com
ATASCADERO, California -- In Monterey County Jail, in the spring of 1981, a 21-year-old drug dealer and junkie named Toby Govea lay in bed shaking violently and uncontrollably. Thanks to a bad batch of homemade heroin, Govea had developed symptoms of Parkinson's Disease, an incurable neurological illness that causes muscle rigidity, tremors and eventually loss of movement.
Today, Govea remains incarcerated -- but free of tremors, thanks to a treatment made possible by research on the prisoner's own brain.
The treatment, called deep brain stimulation, has become the leading surgical treatment for Parkinson's, which afflicts 1.5 million Americans. It has been performed on more than 20,000 patients in the past decade.
In July of this year at the Atascadero State Hospital in California, Govea was lucid, and his muscles were still, as he recalled the events that made him a human guinea pig who helped develop a treatment for his own illness.
As I create this post, I am leaving the errrors that my Parkinson's diease creates through my tremors. This is tod emonstrtae how debilitating the condition can be, espcially to one who writes for a liviingg or as an avocation. Articles I submit fofr publicattion have too be meticuloussly edited before submissioon.
There was a time when my L-Dopa/Carbidopa controlled my symptoms for six hours at a time. Since I took it four times a day, that meant an absence of tremors for 24 hours a day. Now themedicaation works about four hours at a time, leaving me with two hours of significant symptoms -- severe leg a nd arm tremors, difficulty swallowing and ambulating, legs freezing when I walk, especially turing corners and arms freezing when I try to hang clothes in the closet.
Right now I am undegoing EECP for my coronary artery disease. I fear this therapy, which h as signficantly lessened my angina symptoms may be contributingn too my Parkinson's symptoms. I guess I won't know until the therapy is completed next month and I check in with my neurologist back in Indiana. I will keep you posted.
Monday, September 10, 2007
10th EECP Session
When my cardiologist, Dr. Ken LeClerc, examined me before I started EECP, he told me after the 35 consecutive hour-long sessions, he may be able to take me off of some of the medication. I asked if that might mean I could stop taking my beta-blocker and could begin using Viagra or Cialis again. He told me I may not need those drugs to maintain an erection after EECP.
Now as I said above, this feeling may be psychological on my part, but since starting EECP, I have gotten an erection during almost each therapy session. I also am happy to report I have been able to function more than adequately the few times I have engaged in intercourse since beginning EECP.
This therapy, in my opinion, is a logical substitute for coronary artery bypass surgery. It is far less expensive and dangerous as the surgical alternative, not to mention less traumatic to the body. EECP has virtually no contraindications and the side effects are limited to some chafing of the skin, which I have yet to experience.
Anyone who takes the time to read this entire blog from beginning to end will realize I have taken a careful and studied approach to treating my own coronary artery disease and angina. I refused to allow an invasive cardiologist, whom I consider a medical terrorist, to coerce me into getting a quintuple bypass. The medical approach prescribed by Dr. Howard Wayne gave me three years without having to recover from surgery.
Now I have chosen EECP to treat my returned angina symptoms. This therapy, much like Wayne's medical approach, assists the body in creating natural bypasses around clogged arteries. I should enjoy another four to five angina-free years and EECP is a noninvasive treatment that can be performed in a year if necessary. The surgery that the medical terrorists tried to coerce me into in my 56th year, may not need to be done until I am 65 or 69 if lucky.
If you have a greedy cardiologist trying to scare you or your loved ones into bypass surgery, please seek out a second opinion from a noninvasive cardiologist. What do you have to lose?
Thursday, August 30, 2007
EECP & Me
Velcro-secured wraps are placed securely around the legs and lower torso. They squeeze your body every time the heart is at rest. Yesterday Daphne took the pressure up to 6 psi, the maximum therapeutic level.
All of the literature says not to expect to feel any positive results until you have completed around a dozen of the 35 sessions. Well, it may be my imagination, but my tolerance for exercise seems much better and I have had to use nitroglycerin twice since Monday.
It has been a long arduous road from the time I decided to take charge of my own body in 2004. In April of that year, an Indianapolis cardiologist characterized me as a walking time bomb (see the beginning of this blog for more information) unless I had a quintuple coronary artery bypass. I got a second opinion and the rest is history.
To recap, it has been more than three years since I declined to receive the bypass. The EECP will give me another 4 to 5 surgery-free years. That means my life will maintain some semblance of untraumatic normalcy for a total of 8 to 9 years.
American doctors, especially invasive cardiologists and their cardio-thoracic surgeon allies are too quick to cut. Their decisions re based more on the personal finances of the physician and the greed of the hospital they work in.
I agree with the late Dr. Howard Wayne's label of these doctors as "Medical Terrorists." I sincerely believe they use their license to practice medicine as a license to commit assault with a deadly weapon. What else would you call unnecessary invasive surgery you are coerced into receiving?
Thursday, August 16, 2007
Orientation
The first thing I did was watch a video that gave me an overview of what EECP is, how it is performed, expected results, etc. It wasn't anything i hadn't already studied about, but the presentation, produced by the manufacturer of the equipment used in doing EECP, was professionally done and accurate.
Next, we filled out some questionaires regarding symptoms and Daphne fitted me for a pair of tights which are worn when receiving EECP. I will return to the clinic on Monday 20 August for my first session. Patients usually don't feel any results the first ten or so sessions, but I will report how mine went whenever there is something interesting happening.
Wednesday, August 08, 2007
My EECP Begins Soon
I arrived in the Alamo City last Friday to continue the search for someone who will prescribe a course of EECP. I started in Indianapolis where the cardiologists who would prescribe it also required an angiogram. Anyone who has read my site knows what I think of angiograms.
The only tests Dr. LeClerc required were vital signs and an EKG. He does want copies of all the lab work my primary care physician in Indianapolis has in my records.
I should begin my EECP on Monday, 13 August. It takes 35 sessions over seven weeks to finish the therapy, but there is an at least 85% chance it will be successful and my angina symptoms will be controlled for at least five years.
It was a little more than three years ago I started on the late Dr. Howard Wayne's medical regimen. If indeed EECP gives me five more years, I will have lived eight years longer than the cardiologist who wanted to subject me to a quintuple bypass in 2004 said I would.
Sunday, July 29, 2007
Letter
Hello Jeff,
I was reading your blog today. I´m sorry to know that Dr. De Vries is leaving his practice.
And I´m sorry that every doctor wants to do an invasive test in order to prescribe EECP to you.
We are also still seeking a real noninvasive Cardiologist, we haven´t find one yet. Every potential doctor does not want to hear about anything but CABG for my husband.
All this is almost unbelievable :-( , but sadly very true not only in the USA, but at least in Mexico too.
Have you talked to Gypsy? We talked to her last February. she said she was actively trying to find someone interested to buy Dr Wayne's practice. We haven´t heard from her since then.
I´m constantly searching information in the Internet, I ´ve found a few doctors that call themselves noninvasive.
I have not talked to any of them, so I don´t know how true is that. I want to share their names with you, probably you already know them. Maybe one of them can help you.
I was thinking that probably this Dr. Chung could prescribe you the EECP treatment. I don´t know anything else about him than what he has posted in that Cardiology forum, but at least he says he would respect the patient decisions.
There is also this noninvasive center that prescribes EECP: http://whitakerwellness.com
Another noninvasive Cardiologists: Dr. Thiak: http://www.drthaik.com/ , Dr. Gould : http://www.uth.tmc.edu/pet/ , Dr. William R. Davis http://heartscanblog.blogspot
My best wishes in your search.
Best regards from Mexico City.
Maria
EDTA vs EECP
| Originally Posted by Cannuck Chelation has been used for many decades for a variety of reasons. My wife's Aunt was treated with EDTA for the aftereffects of the concentration camps, as were German citizens from the Ruhr Valley for heavy metal poisoning. I personally know seniors who have done so here for various cardiovascular conditions (most with significant success), and can tell you that the results are VERY short in coming. |
When I said EDTA (Chelation therapy) either oral or IV is controversial, that doesn't mean I disapprove of it. Quite the contrary, I feel it is a choice of treatments that has been effective in treating CAD and some other coronary diseases and despite the fact it hasn't been approved by the FDA for use in such diseases, should be available to patients making informed choices. The reason I am opting for EECP is because I have studied its effects, side effects and contraindications and have talked with patients who have received it. Unlike bypass surgery "victims" and angioplasty (balloon & stent) recipients, none of them had negative reports of their experiences.
Further, angiogenesis and the development of a collateral vessel system to naturally bypass the clogged coronary arteries is a process the body already has started on its own, without the introduction of any drug. Like it or not EDTA is a drug and therefore could have side effects or be harmful. There are reports of unexpected deaths during or following chelation therapy. I have found none associated with EECP. That is not to say EECP recipients haven't died as a result of therapy, there simply are no reports where the therapy caused the deaths, that I have found.
I realize EDTA is a natural enzyme and as such can be sold as a nutritional supplement and I am not opposed to nutritional supplements as long as they are used wisely and in some form of a therapeutic regimen. I personally take the following supplements daily in the strengths and doses indicated:
Organic Flaxseed Oil 1200 mg, three times a day
Borago Seed Oil 1200 mg, three times a day
Omega 3 Fish Oil 1200 mg, three times a day
d-Alpha Tocopheryl (Vitamin E) 400 IU, one time a day
Glucosamine 750 mg Chondroitin 600 mg, twice a day
Folic Acid 800 mcg, one time a day
B-100 Ultra B-Complex, one time a day (Puritan's Pride Brand)
l-Arginine 500mg, one time a day
Super C Complex 1000 mg, three times a day (Puritan's Pride Brand)
Acetyl L-Carnitine 400 mg with Alpha Lipoic Acid 200 mg, one time a day
Natural Selenium 50 mcg, four times a day
Co-Enzyme Q10 100 mg, one time a day
Magnesium Oxide 400 mg, one time daily
Multiple Vitamin, one time daily
I always try to take my supplements with food and I am on a schedule that has me taking something, prescribed medications and supplements every six hours.
Just for the information to folks with CAD and angina, my medical treatment regimen is aimed at not only controlling my blood pressure, but keeping it as low as possible without adverse side effects. I try to keep mine around 90/50 when I am at rest. It usually ranges between 80/40 to 100/50. When my BP is a normal 120/70 or more, during stress or increased physical activity, I often experience symptoms of angina. Here are the prescribed drugs I am on daily
Aspirin 325 mg in the morning
Fosinopril
Metopropolol Tartrate
Isosorbide Mn
Nitroglycerine (as needed)
No dosages are provided because you need to consult a physician before starting this protocol. Suffice it to say, some of the dosages are higher than usually recommended. The Isosorbide and Nitroglycerine were recently added to my regimen and Modiuretic was discontinued due to an abnormal increase in blood tests that indicated my liver was being adversely affected. I also take prescription medication for Parkinson's disease.
I cannot emphasize enough the need to be under the care of a medical doctor who you trust and have a good working relationship with. I encourage anyone who has CAD or angina or has a loved one who does to read my blog from beginning to end and to get a second opinion from a non-invasive cardiologist before being coerced into bypass surgery they do not need.
Saturday, July 28, 2007
One More Opinion About EECP

A noninvasive procedure for treating angina has proven nearly as effective as angioplasty, said a cardiologist who has been using Enhanced External Counterpulsation for his patients for the past several years.
Dr. James P. O’Neil, a cardiologist with the Cardiology Group, which administers the procedure at its Mount Laurel office, said coronary angioplasty, a medical procedure which involves inserting a balloon catheter to open a blockage in an artery, and the EECP offer patients “about the same success rate.”
During EECP, cuffs similar to blood pressure cuffs that have been wrapped around patients’ legs are inflated and deflated, forcing blood to flow through arteries. “The body reacts by improving collateral blood flow” with small capillaries expanding to compensate for the blocked artery, said O’Neil.
He said the aim of both procedures is to “improve exercise tolerance and fatigue,” common problems for heart patients.
Angina is a symptom related to coronary heart disease. Blockages in coronary arteries created by the buildup of plaque on the inner walls of the vessels limit the supply of oxygen-rich blood to the heart and cause the chest pain or discomfort known as angina and shortness of breath.
O’Neil said medications are usually the first step in an attempt to ease the discomfort, but if they do not work, then cardiac bypass surgery, angioplasty or EECP treatments should be considered.
He said EECP relieves symptoms in 75 percent of cases, “a little bit less than angioplasty,” which eases symptoms in 80 percent of cases. Cardiac bypass surgery improves symptoms 90 percent of the time, said O’Neil.
O’Neil said The Cardiology Group, which has five offices in Burlington County, has done nearly 300 of the lower risk EECP procedures since it began offering EECP six years ago. The procedure is administered the same now as when it was introduced, in one-hour sessions five days a week for seven weeks.
The time commitment is the only disadvantage of using EECP, said O’Neil, who cited several advantages of using it instead of angioplasty to relieve angina.
“Angioplasty is three times the cost as the EECP, the risk is higher, there is no survival advantage of angioplasty over EECP,” said O’Neil.
O’Neil said a report issued during a recent American College of Cardiology conference supported the view that the two procedures offer similar success.
“We used to think that people lived longer (by having angioplasty),” he said. “Angioplasty is really stretching the vessel and really tearing the vessel. During angioplasty, that vessel is damaged and as it heals, it can cause a scar.”
The resulting scar can create a new blockage, although a drug-eluding stent sometimes is used to hinder the scar buildup, he said.
“One out of 10 patients tend to block up again with that artery,” he said. “With EECP, we’re not damaging an artery and causing scar tissue to build up.
“The big thing that has been found with EECP, a patient is not going to die any more often than those who have angioplasty. There’s a big misconception that if we do angioplasty it’s going to make them live longer.”
An exception, he said, is that when performed during a heart attack, angioplasty can serve as a lifesaving procedure.
O’Neil compared the effectiveness of the three procedures used in relieving angina. He said cardiac bypass surgery improves symptoms in 90 percent of cases, angioplasty in 80 percent and EECP in 75 percent.
The cardiologist said some insurance carriers, including Medicare, only recommend EECP as a remedy for patients who are not considered candidates for cardiac bypass surgery or angioplasty.
“I and many physicians don’t agree. We think EECP should be offered along with bypass and angioplasty,” O’Neil said. “One of the reasons patients don’t want bypass is they are afraid.”
He said insurance regulations sometimes deter patients from taking advantage of EECP.
“One of the biggest obstacles is how the insurance companies can make it difficult. They can and do make it difficult for patients to go through this,” said O’Neil, noting that out-of-pocket charges such as per-visit co-pays can deter patients from having the treatments.
“They might not have as big an out-of-pocket expense if they take the riskier, higher priced procedure,” he said.
O’Neil said EECP costs $6,000 to $7,000 whereas the angioplasty costs $20,000 to $30,000.
Patients who have had EECP say they are happy with the results.
That includes the Cardiology Group’s first EECP patient.
At 83, Nick Russo still mans a tractor to cultivate the pumpkin patch at the family farm in Chesterfield. In March 2001, he was the first patient to undergo EECP at the Cardiology Group.
Although Russo stashes a bottle of nitroglycerin pills in his pocket — just in case — the Westampton man said he hasn’t needed any of the medication since 2003, when a second round of EECP treatments seemed to ease the lingering angina.
Russo, who was diagnosed with a heart problem 10 years ago, underwent an open heart procedure at Deborah Heart and Lung Center in Browns Mills, Pemberton Township, in 1999. He took nitroglycerin to ease angina, eventually deciding to have the EECP.
Russo said his initial EECP treatments were “a little frightening at first. You get a shock.”
After having the EECP in 2001, Russo said, “I would still get out of breath. Once in awhile I would have to take a nitro pill.”
He said he noticed the angina “when I would do anything that was exertion” — lifting bags of fertilizer, loading crates of corn — and his cardiologist suggested a second set of treatments.
Marlene Donnelly of the Cardiology Group said EECP can be repeated “as long as it’s medically indicated.” She said one patient has had three sessions of EECP.
Angioplasty also may be repeated, Donnelly said.
After having a second angioplasty last July (the first was in May 2006), Edward Stickel of Delanco “felt better for a while, and then I started to experience unstable angina. For about 11 consecutive days in September and October I had angina in my left shoulder,” he said.
Stickel, 68, said cardiologist Samuel Ventrella thought EECP would help. He started the treatments on Nov. 6, and after about 12 sessions “started to feel much better.” By Dec. 6, “I stopped having the angina,” said Stickel, who retired from teaching at Palmyra High School, where he also coached freshman football for 18 years. He enrolled in the Cardiology Group’s rehab program, and exercises at the Mount Laurel center twice a week.
The former educator also said he is still able to go waterfowl hunting and fly fishing.
Stickel said he is covered by Medicare and by a Blue Cross/Blue Shield plan and was not troubled by the cost of the EECP treatments.
“I was charged a $5 co-pay, which I found to be not a real problem,” he said.
Jane Tabone-Yerkes of Pemberton Township, who is covered by a Civil Service insurance plan, said she had no co-pay for her EECP treatments, which she completed on Feb. 5.
Diagnosed with a heart problem 17 years ago, Tabone-Yerkes, 76, said, “I feel wonderful. I can go up the steps, I go up and down and I have no problem.”
Tabone-Yerkes, who had a stent inserted following a heart attack in 2005, said she asked her cardiologist for the EECP after reading about the procedure in a magazine. She said a second bypass surgery was not recommended.
During the procedure, “You are plummeted,” said Tabone-Yerkes, describing the sensation.
“It’s like a boxer socking you in every blood vessel of your body, but it was not hard to take,” she said.
Tabone-Yerkes said her angina, which she felt “down one arm,” “disappeared completely after 15 sessions.
“I felt like I did when I had the bypass 17 years ago,” she said.
A nitroglycerin tablet is part of her daily pill regimen, which also includes medications to control diabetes, high cholesterol and high blood pressure. Tabone-Yerkes, who retired from her job as an accounting technician at McGuire Air Force Base, said a low-fat diet and swimming five laps each morning in her pool helps her stay fit, and she recently joined a fitness center that caters to cardiac patients.
She said EECP was a good choice.
“They used to say it’s the last resort, but I don’t think that’s true,” said Tabone-Yerkes.
(from the Burlington County Times)
Don't Believe Your Cardiologist
Big Dave
No matter how you do it, removing the plaque buildup is the cure to most coronary disease. A pharmacological cure would put a lot of heart surgeons out of business.
Actually that's not so, especially for males over 50. We have an uncanny ability to grow collateral vessels through a process called angiogenesis. Now if you have cancer, angiogenesis is a bad thing. It is responsible for the cancer traveling, becoming malignant. In those of us with coronary artery disease, the process actually helps the growth of collateral vessels. That is why, for the great majority of patients with coronary artery disease, a bypass does more harm than good because it destroys our natural bypass.
Regarding the pharmacological cure: if a cardiologist tries to coerce you into a bypass immediately after you have been diagnosed with CAD, believe me, he doesn't have your best interests in mind. Your interests are far behind the interests of the cardiologist, cardio-thoracic surgeon and his team, the hospital, the therapists, etc. A CABG is the most commonly performed and lucrative cardiac surgical procedure. The American Heart Association and the American College of Cardiologists have both officially stated a CABG should be a last resort, after medication and lifestyle change. Yet, most of these medical terrorists whho try to scare, and usually succeed, into scaring you and your wife into having your chest split open, will use every trick in the book to make you think a heart attack, stroke or death are imminent if you don't have an immediate CABG. That is a bald face lie.
I have challenged these blood sucking scum to debate me on my website or any forum of their choice. They do not even acknowledge the challenge because they know such an event would expose them for the charlatans they are.
That challenge still stands. I am not a physician. I am not even a current medical professional, though I was a nurse in the Army for 20 years and have worked for more than 15 years as a safety officer and senior medic on oil rigs. How about it, you medical terrorists who scare your patients into making your Mercedes and pool payments, care for a debate?
Your EECP Questions Answered
What is Enhanced External Counter-Pulsation (EECP)?
The Cleveland Clinic defines EECP as a treatment for those with symptomatic coronary artery disease, not eligible for standard treatments of revascularization. During EECP, cuffs wrapped around the calves, thighs and buttocks are inflated and deflated, gently but firmly compressing the blood vessels in the lower limbs, increasing blood flow to the heart. EECP may stimulate the openings or formation of collateral vessels to create a “natural bypass” around narrowed or blocked arteries.
The Sanger Clinic further defines EECP as a non-invasive procedure for patients with severe refractory angina… (It) can relieve or eliminate angina in patients who are not candidates for angioplasty or bypass surgery.
How does EECP work?
That’s a good question. EECP is designed to relieve angina by improving perfusion in areas of the heart deprived of an adequate blood supply. The cuffs inflate during diastole, the period when the heart muscle relaxes and the chambers fill with blood. The cuffs inflate sequentially from the calves upwards, resulting in increased pressure in the aorta and coronary arteries. Compression of the vascular bed in the legs also increases the return of venous blood to the heart and increases cardiac output. Patients are customarily treated with EECP for an hour a day for a total of 35 hours.
What is the history of the use of EECP in the USA?
The concept of counterpulsation is not new (it was first introduced in the late 1950s at Harvard), but the computerized technology currently available with EECP makes it a relatively new procedure, introduced less than 10 years ago. As of 2003 it is available in only about 200 centers across the United States.
EECP is used to treat patients with chronic stable angina, coronary artery disease, or high blood pressure. Most recently, the Food and Drug Administration (FDA) has approved EECP for the treatment of congestive heart failure. The treatment may be appropriate for patients who are not eligible for such non-surgical interventional procedures as balloon angioplasty, stent placement, rotoblation, atherectomy, or brachytherapy. It may also be used for patients who do not qualify for such surgical treatment as coronary artery bypass graft surgery.
EECP is not the first-line treatment for angina. Rather, it is reserved for patients who have not achieved good results from medication or interventional management of their symptoms.
EECP may benefit patients with such other medical conditions as erectile dysfunction, kidney disease, eye disease, diabetic neuropathy, and other circulatory disorders. More research is needed to evaluate the outcomes of EECP for these patients.
Are there any contraindications for EECP?
EECP is not recommended for patients who have certain types of valve disease; uncontrolled arrhythmias (irregular heart rhythms); severe hypertension; uncontrolled congestive heart failure; significant blockages or blood clots in the leg arteries; or those who have had a recent cardiac catheterization, angioplasty, or bypass surgery.
Are there any risks or side effects?
EECP is a relatively safe and effective treatment, and few adverse side effects have been reported. The main adverse side effect is chafing (skin irritation from the compression of the cuffs). To reduce or prevent this side effect, patients are instructed to wear tight-fitting cycling pants or athletic tights. Leg pain is another adverse side effect.
What are the normal results?
The benefits of EECP are comparable to the results of angioplasty and coronary artery bypass graft surgery: 80% of patients experience significant improvement after EECP treatment. The largest research study on EECP indicates that after receiving treatment, patients used less medication, had fewer angina attacks with less severe symptoms, and increased their capacity to exercise without experiencing symptoms. EECP improves the patient's sense of well-being and overall quality of life; and in some cases, prolongs the patient's life. Benefits five years after EECP treatment are comparable to surgical outcomes.
The effects of EECP treatment last from three to five years and sometimes longer.
EECP does not prevent coronary artery disease from recurring; therefore, lifestyle changes are strongly recommended and medications are prescribed to reduce the risk of recurrent disease.
What sort of lifestyle changes are we talking about?
These are changes you already have, or should have taken:
- Quitting smoking. Smoking causes damage to blood vessels, increases the patient's blood pressure and heart rate, and decreases the amount of oxygen available in the blood.
- Managing weight. Maintaining a healthy weight, by watching portion sizes and exercising, is important. Being overweight increases the work of the heart.
- Participating in an exercise program. The cardiac rehabilitation exercise program is usually tailored for the patient, who will be supervised by professionals.
- Making dietary changes. Patients should eat a lot of fruits, vegetables, grains, and non-fat or low-fat dairy products, and reduce fats to less than 30% of all calories. Alcoholic beverages should be limited or avoided.
- Taking medications as prescribed. Aspirin and other heart medications may be prescribed, and the patient may need to take these medications for life.
- Following up with health care providers. The patient needs to visit the physician regularly to control risk factors.
Sunday, July 22, 2007
A Letter to the Editor about EECP
Dear (Napa Valley Register ) editor,
This is a belated thanks to Dr. Dizman, Napa cardiologist, and nurse Susan Hart for giving me medical service that changed my life and avoided the problems that come with bypass surgery.
For some time before October 2001, I was suffering periodic chest pains. I finally went to a cardiologist (not Dr. Dizman) who after an examination scheduled me for a bypass operation. Before I had the operation, I went to see Dr. Dizman about his non-invasive heart treatment program, Enhanced External Counter Pulsation.
I canceled by scheduled bypass operation and started the EECP therapy given by nurse Susan Hart. After completing the 35 daily sessions, my chest pains were gone, and I haven’t had any problems since then. I strongly recommend that anyone thinking about getting a bypass operation check out the EECP therapy available at Dr. Dizman’s medical center. If it doesn’t help, you can always get a bypass operation. Medicare paid for the EECP therapy, so it must be an approved medical program.
John J. Eberle / Napa
Seeking a Noninvasive Cardiologist
If you have not read my blog from the beginning, you may not understand why I am so adamant about this. Let me briefly bring you up to date and encourage you to read my entire blog.
In April 2004, I was diagnosed with coronary artery disease (CAD) which I was told was the cause of the angina I had been experiencing for about six months. The interventionalist cardiologist my family doctor sent me to, tried to coerce me into an immediate quintuple CABG, despite the fact, that as he put it, my heart was "in great shape." He wouldn't tell me how my heart could bee in great shape when the arteries that were providing it oxygen were 85 to 100 percent blocked.
He did try to schedule me for the quintuple CABG on Thursday, two days later. When I told him I wanted a second opinion, he told me I was a "walking time bomb," and that I could "have a heart attack, stroke, or even die within three months." I replied that I had been experiencing angina for six months and would take the risk.
I'm glad I did. I sought out the opinion of Dr. Howard Wayne of the Noninvasive Heart Clinic in San Diego. To make long story short, he evaluated me and started me on medical treatment I remain on until this day, three years and four months later.
Unfortunately, in November 2006, the angina returned while I was running to make a connection at Charles De Gaulle Airport in Paris. I contacted Dr. Wayne's clinic and sadly learned he had passed away three weeks earlier. (Lest anyone assume he was the victim of heart disease, Dr. Wayne died while climbing mountains near Lake Tahoe. He was 83.)
I saw a doctor in Chicago who agreed to follow the protocol set up by Dr. Wayne, although he did feel I should have the CABG. He also thought I might benefit from Enhanced External Counterpulsation. EECP is a noninvasive therapy.
My doctor in Chicago is leaving his practice and I can not find a cardiologist in Indianapolis that will prescribe EECP unless I undergo an angiogram. Readers of this blog will understand why that is out of the question.
There may come a time when I will be convinced the medical and noninvasive treatments for my angina and CAD are no longer working and I will undergo a CABG. However, I will not be coerced into what I consider to be unnecessary surgery by people I consider to be medical terrorists who are more interested in making money than properly treating my medical conditions.
Therefore, I am seeking a noninvasive cardiologist to prescribe EECP and follow me during and after the seven weeks of therapy. If you know one, please have him or her contact me at jeff.brailey@gmail.com.
Saturday, July 21, 2007
Your Angiogram Increases Your Cancer Risk
Computed tomography coronary angiography carries a "nonnegligible" risk for cancer, which varies greatly by age and gender, according to a study in JAMA.
The study was based on risk estimates -- developed for the National Academies' Biological Effects of Ionizing Radiation report -- that were applied to simulation models.
The lifetime attributable risk for cancer from a single CTCA for women was 1 in 143 at age 20, 1 in 284 at age 40, and 1 in 466 at age 60. Lung and breast cancer accounted for about 80% of the cancer risk in women.
Men's risks were considerably lower: 1 in 686 at age 20, 1 in 1007 at age 40, and 1 in 1241 at age 60. Women's higher risk was attributed to the greater radiosensitivity of their lungs and to the fact that the breast lies in the field irradiated during CTCA.
The authors note that CTCA "should be used particularly cautiously in the evaluation of young individuals, especially women."