Friday, January 19, 2007
Uh Oh... we'd better stop doing that!
It's not nice to fool Mother Nature -- It seemed like a good idea, but combining a carotid endarterectomy with a coronary artery bypass graft increased the risk of postoperative stroke and death by nearly 40% over CABG alone, investigators reported.
In a review of records on patients nationwide who underwent CABG with or without carotid endarterectomy, the odds ratio for a combined endpoint of postoperative stroke or death was 2.25 for patients who underwent both procedures, reported Richard M. Dubinsky, M.D., M.P.H., and Sue Min Lai, Ph.D., M.B.A., of the University of Kansas Medical Center.
After correction for co-morbidities, the odds ratio was reduced to a smaller but still significant 1.38 compared with patients who underwent CABG only, they wrote in the Jan. 15 issue of Neurology.
Their findings suggest that theoretical benefit of combining the surgeries may not outweigh the increased risks.
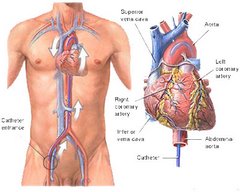
"The underlying rationales for combined carotid endarterectomy-CABG are to protect the carotid circulation from artery-to-artery embolic stroke during CABG and to lessen the risk by having just one operation, albeit longer, and one exposure to anesthesia," the authors wrote.
"Although there is an increased likelihood of carotid artery disease in those with coronary artery disease, the risk of asymptomatic carotid artery stenosis is low enough that perioperative mortality can be greater than the benefit of reduced risk of stroke compared with medication alone."
The investigators conducted a retrospective study of records from the Nationwide Inpatient Sample, a database that provides yearly admission and discharge data from nearly 1,000 hospitals.
They extracted data on community-wide mortality and morbidity rates in patients undergoing combined carotid-endarterectomy-CABG in the United States from 1993 through 2002.
The cohort included 657,877 patients ranging from 32 to 89 years old, 178,959 of whom underwent endarterectomy alone, 471,881 who underwent CABG alone, and 7,037 who underwent both procedures. Of the combined surgery group, 1,203 were known to have undergone the procedures on the same day; the spacing of procedures in the remaining 5,807 was unknown.
The investigators calculated the odds ratio for the combined outcomes of postoperative stroke or death for same-day endarterectomy-CABG to be 2.16 (95% confidence interval 1.78 to 2.62, P<0.0001) compared with CABG alone, and for those patients in whom the spacing of the procedures was unknown the odds ratio was 2.28 (95% CI 2.08 to 2.48, P<0.0001). For all combined procedures the odds ratio was 2.25 (95% CI 2.08 to 2.44, P<0.0001).
There were no changes over time in the rate of postoperative stroke or death in the combined surgery groups, the authors noted.
In a logistic regression model of those older than 65, procedures performed in urban non-teaching hospitals, and co-morbidities (Charlson index score > 1) were also associated with increased risk for in-hospital death and postoperative stroke, with female sex being the only factor associated with lower in-hospital mortality for people undergoing both procedures.
"The logistic regression models confirmed that for combined carotid endarterectomy-CABG, the higher risk persisted even after controlling for all risk factors and remained unchanged when individual comorbidities (rather than the co-morbidity index) were analyzed," the investigators wrote.
The adjusted odds ratio for the combined endpoint of postoperative stroke or death was 1.38 (95% CI 1.27-1.50, P<0.0001).
The authors noted that the increased risk seen with the combined procedures might be attributable to residual confounders, such as previous stroke or the degree of carotid artery stenosis.
They also acknowledged that the administrative data they relied on could include diagnostic coding errors and omissions of some co-morbidities. Their analysis could not account for the degree of carotid stenosis, extent of previous strokes, use of pre-operative medical therapies, or physician experience.
"The frequency of combined carotid endarterectomy-CABG has increased, but the reported case series are inadequate to conclude whether there is a benefit to combining the procedures," Dr. Dubinsky and Dr. Lai wrote. "A randomized controlled clinical trial, stratified for the degree of carotid stenosis and for previous stroke, with a follow-up of at least one year, is clearly needed to determine the benefit, if any, of combined carotid endarterectomy-CABG in patients with carotid and coronary atherosclerosis."
This just goes to show you that surgical procedures should be approved by an entity like the FDA before being introduced into use on the general population. How would you like to be or have had one of your loved ones be one of that 40%?
At the very least, cardio-thoracic surgeons should:
1. tell the patient studies show when the CABG and carotid endarterectomy are performed together, there is about a 40% higher risk of stroke or death after surgery than for CABG alone.
2. point out that not all co-morbidities could be determined in this study and a randomize, controlled trial would be necessary to determine the benefits of lack of benefit of this procedure.
In a review of records on patients nationwide who underwent CABG with or without carotid endarterectomy, the odds ratio for a combined endpoint of postoperative stroke or death was 2.25 for patients who underwent both procedures, reported Richard M. Dubinsky, M.D., M.P.H., and Sue Min Lai, Ph.D., M.B.A., of the University of Kansas Medical Center.
After correction for co-morbidities, the odds ratio was reduced to a smaller but still significant 1.38 compared with patients who underwent CABG only, they wrote in the Jan. 15 issue of Neurology.
Their findings suggest that theoretical benefit of combining the surgeries may not outweigh the increased risks.
"The underlying rationales for combined carotid endarterectomy-CABG are to protect the carotid circulation from artery-to-artery embolic stroke during CABG and to lessen the risk by having just one operation, albeit longer, and one exposure to anesthesia," the authors wrote.
"Although there is an increased likelihood of carotid artery disease in those with coronary artery disease, the risk of asymptomatic carotid artery stenosis is low enough that perioperative mortality can be greater than the benefit of reduced risk of stroke compared with medication alone."
The investigators conducted a retrospective study of records from the Nationwide Inpatient Sample, a database that provides yearly admission and discharge data from nearly 1,000 hospitals.
They extracted data on community-wide mortality and morbidity rates in patients undergoing combined carotid-endarterectomy-CABG in the United States from 1993 through 2002.
The cohort included 657,877 patients ranging from 32 to 89 years old, 178,959 of whom underwent endarterectomy alone, 471,881 who underwent CABG alone, and 7,037 who underwent both procedures. Of the combined surgery group, 1,203 were known to have undergone the procedures on the same day; the spacing of procedures in the remaining 5,807 was unknown.
The investigators calculated the odds ratio for the combined outcomes of postoperative stroke or death for same-day endarterectomy-CABG to be 2.16 (95% confidence interval 1.78 to 2.62, P<0.0001) compared with CABG alone, and for those patients in whom the spacing of the procedures was unknown the odds ratio was 2.28 (95% CI 2.08 to 2.48, P<0.0001). For all combined procedures the odds ratio was 2.25 (95% CI 2.08 to 2.44, P<0.0001).
There were no changes over time in the rate of postoperative stroke or death in the combined surgery groups, the authors noted.
In a logistic regression model of those older than 65, procedures performed in urban non-teaching hospitals, and co-morbidities (Charlson index score > 1) were also associated with increased risk for in-hospital death and postoperative stroke, with female sex being the only factor associated with lower in-hospital mortality for people undergoing both procedures.
"The logistic regression models confirmed that for combined carotid endarterectomy-CABG, the higher risk persisted even after controlling for all risk factors and remained unchanged when individual comorbidities (rather than the co-morbidity index) were analyzed," the investigators wrote.
The adjusted odds ratio for the combined endpoint of postoperative stroke or death was 1.38 (95% CI 1.27-1.50, P<0.0001).
The authors noted that the increased risk seen with the combined procedures might be attributable to residual confounders, such as previous stroke or the degree of carotid artery stenosis.
They also acknowledged that the administrative data they relied on could include diagnostic coding errors and omissions of some co-morbidities. Their analysis could not account for the degree of carotid stenosis, extent of previous strokes, use of pre-operative medical therapies, or physician experience.
"The frequency of combined carotid endarterectomy-CABG has increased, but the reported case series are inadequate to conclude whether there is a benefit to combining the procedures," Dr. Dubinsky and Dr. Lai wrote. "A randomized controlled clinical trial, stratified for the degree of carotid stenosis and for previous stroke, with a follow-up of at least one year, is clearly needed to determine the benefit, if any, of combined carotid endarterectomy-CABG in patients with carotid and coronary atherosclerosis."
This just goes to show you that surgical procedures should be approved by an entity like the FDA before being introduced into use on the general population. How would you like to be or have had one of your loved ones be one of that 40%?
At the very least, cardio-thoracic surgeons should:
1. tell the patient studies show when the CABG and carotid endarterectomy are performed together, there is about a 40% higher risk of stroke or death after surgery than for CABG alone.
2. point out that not all co-morbidities could be determined in this study and a randomize, controlled trial would be necessary to determine the benefits of lack of benefit of this procedure.
Subscribe to:
Post Comments (Atom)







No comments:
Post a Comment