Thursday, November 30, 2006
Almost December
Nights, when I am at rest, the picture changes. The BP usually stays around 90/50, but sometimes falls as low as 86/40. My pulsed when supine is a slow 52 or so. I don't sleep very well, a combination of old age, the increased need to empty my old bladder several times a night and frequent leg cramps that happen after I've been in bed about four or five hours.
Well, I head home in three weeks and will spend Christmas & New Years in the USA before returning back to Nigeria. Before I come back, I do have an appointment with a new noninvasive cardiologist in Chicago. I hope he is half as good as Dr. Wayne was.
Sunday, November 26, 2006
Update #1
and half a dose (50mg) at 1:30 PM. A few instances of minor chest pain that I am reluctant to even categorize as anginal bothered me a bit throughout the day. I forgot to bring my BP cuff to work so I don't know what it's running. I'll bring it tomorrow.
Book Review
|
| |||||||||||||||
| ||||||||||||||||
Saturday, November 25, 2006
Twenty Eight Months Ain't Bad
A month or so ago, I noticed my blood pressure was beginning to stay about ten points higher than the 90/50 my medication had been keeping it at rest. Then, I had a minor bout of angina while rushing through Charles de Gaulle Airport near Paris. It went away as quickly as it started after I sat down for a few minutes. Since then, I have increased my metapropolol slightly, taking 100mg in the morning, 50mg mid day and 100mg at night. I just started the increased dosage a couple of weeks ago and, to tell the truth, have not been as faithful in taking my medications on time as I should have been.
This morning, I took my cardiac meds at about 8:30 AM. At 1:00 PM, I climbed some stairs and began walking around the deck of the oil rig I work on. The angina started pretty soon after I began my walk and started subsiding when I returned to my office. My blood pressure cuff is in my cabin and I don't want to wake my cabin mate, so I'll forgo measuring it until this evening. Yesterday evening it read 86/51. I just took half a 100mg Metapropolol about 1:20 PM. It is now 2:00 PM and I am back to normal.
I have made an appointment to see a noninvasive cardiologist in Chicago on January 9, 2007. Until then, I'll continue to monitor my BP and titrate my medications to control any further angina attacks. I think I'll record events related to the return of my unstable angina here on the blog, so you will probably see a lot more activity here for a couple of months.
I still am sold on the idea that medication regimens should preclude angioplasty and CABG, which should be a last resort. I know I made the right decision to opt for the medical treatment instead of the surgical. If I had my chest cracked open in June 2004, I never would have been able to land this very lucrative job I have.
I am convinced I will get through this resurgence of angina and stave off the scapel for at least the forseeable future. More tomorrow.
Sunday, November 19, 2006
Angiograms - Most Useless Diagnostic Tool
These were completely normal assumptions -- for 1958. However, as time went on and more and more patients underwent angioograms and the fidnings were correlated with the patient's symptoms, my cardiologist began to realize these assumptions were not all true. For example, one study involved a group of United States Marine runners who were selected for their endurance. These subjects all had normal stress tests and were made to undergo angiograms. One could not conduct this kind of study on civilians because there was no justification for performing such tests. To everyone's surprise, a substantial proportion of the Marines had significant coronary artery disease. In some, the disease was so severe they were made to stop running. Why did they not have symptoms?
Marathon runners are occasionally known to drop dead suddenly. It has always been assumed the stress of running was responsible. However, my cardiologist remembers a study he was doing with these recording techniqiues on a running team. He was trying to correlate cardiac function with the runners' performances. To his surprise, a number of runners had impaired cardiac function. Since this was a research study, my cardiologist was not allowed to say anything. One day, he received a call from the team's physician, who was also a runner, asking what my cardiologist had fund on a particular runner. In checking the recordings, he informed the doctor that by his assessment, the function of the heart was considerably impaired. When my cardiologist asked the doctor why he wanted to know, he replied both he and the individual in question had both run marathons the week before without any problems. Tragically, the runner had been found dead in bed a few days later and the autopsy had showed severe CAD.
Similar studies had been carried out onn apparently healthy subjects with normal EKGs, but who had abnormal stress tests. These individuals were made to undergo angiograms. A surprising number of such "healthy individuals" turned out to have severe CAD in several vessels. Yet most were extremely active, even running and playing tennis without symptoms. How could that be? Indeed, some had complete obstruction of a coronary artery, yet there was no history of heart attack and their EKGs were entirely normal.
There is a lack of correlation between angiogram findings and symptoms. Some patients have had repeat and serial angiograms done. If CAD were the cause of their symptoms, then one would expect that in patients whose symptoms had progressed, their CAD would have also progressed. But most of the time, there was no change in their disease. Conversely, it was anticipated that in patients whose symptoms had not changed, or even improved, that their coronary artery disease would have remained stable or even improved. Surprise, that, also, was not the case. Their CAD was often actually worse. Could it be there were other reasons, beside CAD, that these patients were having chest pain?
The biggest mystery to my cardiologist came from studies in which the patiengt had narrowing in two coronary arteries, one mild and one severe. These were the ones that were usually rushed into the OR because the severely narrowed coronary artery was expected to close off at any minute. Instead, these patients were followed for several years until they had a heart attack and the angiogram was repeated. Everyone had suppposed that the most severely narrowed artery would have been the one that had completely obstructed. Instead, it was found that in most cases it was the coronary artery that was only mildly narrowed that had closed off and caused the heart attack. What was going on?
So enamored were cardiologists and surgeons with the angiogram, and the money such tests brought in, that in spite of these wide gaps in what the angiogram was reported to show, there was almost no attempt to explain these discrepancies. It was frightening, because if yousubdivided groups of patients with CAD into those who had no symptoms, those that had symptoms that had been present for years but were unchanged, those with sympptoms that were getting worse, those who were about to have a heart attack, those who just had a heart attack and those who were about to die, and gave their angiograms to any cardiologist, and asked him to organize the angiograms and place each in its approrpriate group, HE WOULD NOT BE ABLE TO TELL ONE FROM THE OTHER! He couldn't even tell who was having chest pain fom the angiogram!
How then, can a cardiologist decide who needs bypass surgery and who does not, if he can't tell from the angiogram whether the patients' disease is coming or going?
The angiogram fails to provide any information about the multitude of small coronary arteries that supply blood to the heart.
The angiogram fails to provide information about the function of the heart muscle since cardiac muscle can't be imaged by x-ray.
Angiograms are one of the most useless, but profitable tools your cardiologist uses.
Friday, November 10, 2006
Dr. Wayne & Me
My primary care physician had sent me to a cardiologist after I presented with complaints of chest tightness and shortness of breath on exertion over the past several months. The cardiologist ran a stress test and took some pictures of my heart then said I needed an angiogram. Before becoming fully alert following the procedure, that cardiologist and a cardio-thoracic surgeon stood over my bed in the recovery suite and gave me the bad news.
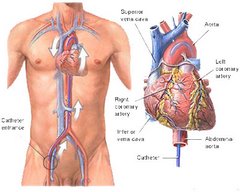
I was told my heart was in great shape but the coronary arteries that supplied it with oxygen sucked. Two were 100% blocked and three others were 85% or more blocked. Under the influence of twilight sleep, administered for the cardiac catheratization done to perform the angiogram, I agreed and a surgery date of Thursday was set. This was on Tuesday.
At no time during this stressful period immediately following the angiogram did either doctor inform me of alternative and less traumatic treatments. I was not informed of the many complications, including heart attack or death, that could occur. I was led to believe that this, most common cardiac surgery, was a piece of cake. It was just a twist of fate that saved me from having my chest cracked opened and my heart stopped while five of my arteries were replaced.
On Wednesday evening, just after I started the pre-operative prep I was told to use the night before surgery, the surgeon's nurse called. It seems he was not in network with my insurance and therefore could not do my bypass. "But wait," I said, "Yesterday I was told I was a walking time bomb that could explode at any minute. I needed an immediate quintuple bypass to prevent a heart attack or worse. Now you are telling me I can't have the surgery because your doctor doesn't accepot TRICARE?"
That was about the size of it. My cardiologist would be in touch with a list of doctors in network. By Thursday, the day my surgery was to have taken place, I was much more alert than when the doctors attempted to railroad me into surgery. I asked the cardiologist how my heart could be so healthy when the arteries that feed it oxygen are so bad. He couldn't give me a good answer, so I did an Internet search for a second opinion.
Despite the urging of my primary care physician and local cardiologist to have the bypass, I decided instead to travel from Indianapolis to San Diego to find out what Dr. Wayne thought. It was probably the smartest move I have ever made. His website had come up in the Google Search I did on "noninvasive cardiology."
Eevn before I made the trip, I realized Wayne was an unusual physician. He actually and personally answered emails within a few hours time. Not only that, he personally called me on the phone to discuss my case. We set an appointment for the following week, on June 4, 2004.
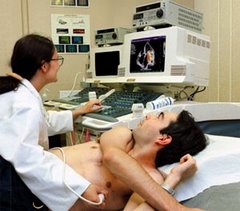
I've been in medicine for going on 40 years, but Wayne's practice was like none I'd ever seen. No technician, no nurse, no receptionist, Just Dr. Wayne and a roomful of modern looking electronic equipment. Dr. Wayne did it all and provided old fashioned, personalized medical care. The entire initial visit lasted a total of about five hours with an hour break for me to eat and him to record the data he had gathered. He patiently answered all questions in an understanable manner and would not let me leave until he was satisfied I understood all of his instructions about my medications.
I learned how collateral blood vessels take over for blocked cornary arteries. I found out about angio-genesis. I found out that my severe coronary artery disease did not cause my angina. It was high blood pressure I didn't even know I had. He was the first doctor to ever measure my BP while at rest and then after a minute of squeezing a grip-measuring instrument while holding my arm in the air. It was 120/70 at rest and 180/130 after one minute of squeezing.
To make a long story short, Dr. Wayne started me on a regimen of a beta-blocker, ace inhibitor and diaretic in June of 2004. I was free of all angina until about a week ago. Since then, I have adjusted my medication dosage and have had no problem. I am seeking a noninvasive cardiologist to take care of me and I hope I can find one in Indiana.
Do You Really Need Bypass Surgery? A Second Opinion
Each year over two million patients undergo coronary angiograms, coronary bypass surgery, angioplasty, or have stents inserted into their coronary arteries. The vast majority undergoing these intervengtions are INCORRECTLY that these procedures must be performed immediately and that, without recommended intervention, they are at great risk for a heart attack.
Rarely is the patient provided with TRUE INFORMED CONSENT about the high rate of complicvations in such surgery, including heart attack or death, or that there are OTHER OPTIONS for both diagnosis and treatment that are far safer, more effective and less costly. The expense of all this effort, as well as the number of lives lost, is staggering.
Yet, simply put, bypass surgery and the insertion of stents are OBSOLETE. Accordingly, all of these procedures are unnecessary. Worse, they are responsible for over 35,000 DEATHS, 65,000 HEART ATTACKS and a whole host of surgical complications a year.
In contrast, modern therapy with FDA approved drugs and guided by modern, noninvasive imaging technology, can transform heart problems due to coronary artery disease into a BENIGN ILLNESS with a normal life span. In short, heart attacks and premature death from coronary artery disease can be prevented in patients without surgery.
This information may seem unbelievable and startling to many of you. But it can be found, with documentaion from reputable medical authorities, in Howard Wayne's new book, DO YOU REALLY NEED BYPASS SURGERY? A Second Opinion. Dr. Howard Wayne, M.D., M.S., F.A.C.C.,F.C.C.P., and F.A.C.P., was the director of the Noninvasive Heart Center of San Diego until his untimely death on October 23, 2006. He would have been 83 years old a few weeks after his death, which occurred while on vacation with his family at Lake Tahoe.
The book documents Dr. Waynes' radical statements with over 360 references from the medical literature. It describes how this cardiologist, with a full time practice, who sent many patients for angiograms and bypass surgery in the earlier years of his career, to someone who did not send a patient for surgery during the last 11 years of his practice. His patients almost never have heart attacks and the vast majority are symptom-free.
If you or someone you love have heart disease, this is a must read. This book will save lives. It is available from this website: www.heartprotect.com
Wednesday, November 01, 2006
Howard Wayne
Dr. Wayne obtained a combined M.D. and Masters degree in cardiovascular physiology at the Bowman Gray School of Medicine at Wake Forest and received his training at the Cleveland Clinic. Early in his career, while on the Faculty of the United States Air Force School of Aerospace Medicine, the forerunner of the National Aeronautics and Space Administration (NASA), he was challenged by the frequent occurrence of unexplained accidents involving high performance aircraft. In addition, criteria were being defined for the selection of future astronauts. (It wouldn't due for an astronaut to have a heart attack on the moon or halfway between Earth and Mars). Because the conventional cardiac evaluation, which is still used today, was so insensitive in the detection of heart disease, the thinking at that time was that supposedly healthy pilots were having heart attacks. Consequently, one of his early interests was to discover new ways of uncovering heart disease in pilots and future astronauts. This started him on a career long quest of an early warning system so that heart disease not only could be diagnosed but treated as early as possible.
With grant support from the American Heart Association, Dr. Wayne was successful in applying new methods to study heart function and to use these procedures to uncover heart disease long before traditional examination methods. Subsequently he wrote the first textbook on noninvasive cardiology in the early seventies. During the seventies and eighties Dr. Wayne set up scientific exhibits and gave lectures throughout the United States, Europe and Asia to teach other doctors about these new methods of examination. From 1975-1979 his scientific exhibits were displayed on multiple occasions at annual meetings of the American College of Cardiology, the American Heart Association, the American College of Physicians, the American College of Chest Physicians, the American Medical Association, the European College of Cardiology and the Asian Society of Cardiology. His scientific exhibit won the American Medical Association's first prize in 1975. In the process of detecting heart disease prior to the appearance of symptoms, he was able to discover more effective ways of treating coronary heart disease with medication.
The combination of early detection and treatment has been so successful that only eleven of his patients have had to undergo coronary artery bypass surgery or angioplasty in the past 22 years. In addition, heart attacks and premature death have become exceedingly rare in the patients who remain on a tailored medical program. Dr. Wayne feels strongly that heart disease need not be the number one killer it is today. With proper and early diagnosis with modern noninvasive tests, and appropriate treatment with up-to-date drugs, it can be turned into a benign disorder compatible with a good quality of life and a normal life span. Heroic procedures such as angioplasty and bypass surgery are only rarely necessary. Doctors who quickly urge patients to have these treatments as soon as symptoms appear may be more dangerous to the patient than their disease.