Wednesday, December 15, 2004
Year is almost over
In 15 days we will end 2004 and start a new year. This has been an interesting year for me, one of health problems that required major decisions. I was told in April that I needed a quintuple coronary artery bypass. This information was presented to me in such a way that I was led to believe I would never see 2005 unless I let a cardiothoracic surgeon crack my chest. Well, I opted for a second opinion, decided to be treated with medication rather than surgical intervention and am I ever glad I did.
I began my medical regimen In June. Now, half a year later, I can honestly say I have not had any symptoms I recognized as the angina that caused me to seek medical help in the first place. I take 22 pills a day, including medication for my Parkinson's Disease and I feel wonderful. Rebecca, the lady in my life and I are in the process of writing a book and all is right with the world.
The reason I am posting this message is to urge anyone who has been told he or she requires heart surgery to get at least a second and maybe a third opinion. And have a great Christmas and a prosperous and healthy new year.
I began my medical regimen In June. Now, half a year later, I can honestly say I have not had any symptoms I recognized as the angina that caused me to seek medical help in the first place. I take 22 pills a day, including medication for my Parkinson's Disease and I feel wonderful. Rebecca, the lady in my life and I are in the process of writing a book and all is right with the world.
The reason I am posting this message is to urge anyone who has been told he or she requires heart surgery to get at least a second and maybe a third opinion. And have a great Christmas and a prosperous and healthy new year.
Saturday, October 30, 2004
Good Saturday Morning
Good morning from the heartland of America. My blood pressure continues to register around 90/50 almost every day and I am completely without angina pain, shortness of breath or any other symptoms of cardiac problems or hypertension. I continue to take my medication as ordered and feel great. I have lost approximately 15 pounds since the summer and continue to eat right and exercise moderately. Except for some morning bach aches, knee pain and occasional neck pain from arthritis and degenerative joint disease every person my age begins suffering, I am in excellent health. I will post my blood pressure and pulse readings from October 7 in a day or two.
If anyone who comes across this blog has any questions or comments, feel free to make them. Have a safe Halloween and don't forget to vote Tuesday.
If anyone who comes across this blog has any questions or comments, feel free to make them. Have a safe Halloween and don't forget to vote Tuesday.
Thursday, October 07, 2004
BP Report 9/7/04 thru 10/7/04
(This is a copy of my BP Report sent to Dr. Wayne today.
My BP Report for 9/7/04 thru 10/7/04 follows:
Date Time BP Pulse
9/07 2100 90/47 60
9/08 2045 105/60 62
9/09 2300 80/46 58
9/10 1100 94/48 66
9/11 2000 102/52 66
9/12 2000 94/54 60
9/13 2015 122/70 62
9/14 2100 96/56 64
9/15 2115 96/56 62
9/16 2000 104/56 86
9/17 1900 104/56 70
9/18 2145 96/54 58
9/19 2130 100/56 60
9/20 2100 102/58 74
9/21 2130 90/50 70
9/22 2145 100/54 66
9/23 2045 104/60 56
9/24 2100 106/56 58
9/25 2045 100/56 64
9/26 2000 104/58 70
9/27 2100 100/60 62
9/28 2000 104/56 72
9/29 2030 94/52 62
9/30 2045 112/68 68
10/1 2045 104/56 66
10/2 1900 104/54 70
10/3 1945 104/56 70
10/4 2045 104/58 64
10/5 1945 94/56 60
10/6 2100 104/54 70
10/7 1230 94/50 68
The lightheadedness his been gone for about a week now. I have noticed my BP is slightly higher than it had been running and I have had a couple of minor occassions of a small amount of chest tightness, not associated with exertion. It may be due to the change in the weather, I do not feel bad at all. When my BP was really low and I was getting a lot of lightheadedness, we cut the monpril from 20mg to 10mg. Should I go back up to 20mg and see what happens?
My BP Report for 9/7/04 thru 10/7/04 follows:
Date Time BP Pulse
9/07 2100 90/47 60
9/08 2045 105/60 62
9/09 2300 80/46 58
9/10 1100 94/48 66
9/11 2000 102/52 66
9/12 2000 94/54 60
9/13 2015 122/70 62
9/14 2100 96/56 64
9/15 2115 96/56 62
9/16 2000 104/56 86
9/17 1900 104/56 70
9/18 2145 96/54 58
9/19 2130 100/56 60
9/20 2100 102/58 74
9/21 2130 90/50 70
9/22 2145 100/54 66
9/23 2045 104/60 56
9/24 2100 106/56 58
9/25 2045 100/56 64
9/26 2000 104/58 70
9/27 2100 100/60 62
9/28 2000 104/56 72
9/29 2030 94/52 62
9/30 2045 112/68 68
10/1 2045 104/56 66
10/2 1900 104/54 70
10/3 1945 104/56 70
10/4 2045 104/58 64
10/5 1945 94/56 60
10/6 2100 104/54 70
10/7 1230 94/50 68
The lightheadedness his been gone for about a week now. I have noticed my BP is slightly higher than it had been running and I have had a couple of minor occassions of a small amount of chest tightness, not associated with exertion. It may be due to the change in the weather, I do not feel bad at all. When my BP was really low and I was getting a lot of lightheadedness, we cut the monpril from 20mg to 10mg. Should I go back up to 20mg and see what happens?
Sunday, October 03, 2004
October Update
Well, at least one reader left a reply to a couple of posts since I began this Blog, so perhaps my story is being read by people who have been told they need coronary bypass surgery and probably really do not. I continue to do well on my medication regimen, however, in the past couple of weeks I have noticed a slight rise in my blood pressure readings throughout the day. Before, I was averaging around 90/50 or slightly lower. Recently, they have been around 100 over 56, not a very perceptible difference, however, I have noticed some occasions of what I would describe as "chest discomfort a couple of times this week. Of course, most chest symptoms people experience are not related to the heart, so I am not really worried about them, especially sense my heart rate continues to be strong and normal.
I also will admit to increased symptoms of arthritic pain, especially in my back and neck, where I have DJD and my knees and shoulder as well. Frankly, I attribute these aches and pains to the changes in the weather the fall brings. This morning, as I type this entry, it is 37 degrees in Brownsburg, Indiana. I already take two aspirin four times a day so I will not take any other pain medication to ease the pain. However, I have become more liberal in the application of analgesic balm. Oh well, I guess I'll send Dr. Wayne an update email tomorrow and see what he says about the blood pressure readings. Until next time,hang in there and enjoy life.
I also will admit to increased symptoms of arthritic pain, especially in my back and neck, where I have DJD and my knees and shoulder as well. Frankly, I attribute these aches and pains to the changes in the weather the fall brings. This morning, as I type this entry, it is 37 degrees in Brownsburg, Indiana. I already take two aspirin four times a day so I will not take any other pain medication to ease the pain. However, I have become more liberal in the application of analgesic balm. Oh well, I guess I'll send Dr. Wayne an update email tomorrow and see what he says about the blood pressure readings. Until next time,hang in there and enjoy life.
Tuesday, September 21, 2004
Returned to My Indiana Cardiologist
Well, I had an appointment with my cardiologist's Physician Assistant this morning and was she ever surprised. Remember, this is the Indiana cardiologist who thought I needed a bypass operation when he last saw me in May.
Now I have been on my medication regimen since June 6, have lost almost 10 pounds,, feel great and look well, too. She was shocked at my low blood pressure (80/50) and took it twice. She was surprised to find my BP rarely goes above 90/50 any more and that my lightheadedness is pretty much gone. She gave me a cursory physical exam, listened to my lungs, heart and abdomen with her stethoscope, asked several questions and then declared that since Dr. Wayne is going to see me once a year, Dr. Cory can do the same. My next appointment is Sept. 26, 2005.
Now I have been on my medication regimen since June 6, have lost almost 10 pounds,, feel great and look well, too. She was shocked at my low blood pressure (80/50) and took it twice. She was surprised to find my BP rarely goes above 90/50 any more and that my lightheadedness is pretty much gone. She gave me a cursory physical exam, listened to my lungs, heart and abdomen with her stethoscope, asked several questions and then declared that since Dr. Wayne is going to see me once a year, Dr. Cory can do the same. My next appointment is Sept. 26, 2005.
Saturday, September 18, 2004
Why we are here...
Well, everyone has to be someplace, every minute of the day. Since wordworks2001 was banned from HealthBoards.com for speaking his mind, I decided to move many of my posts from that site to this blog. Unfortunately, I was unable to replicate my original posting to HealthBoard, which was titled "My Experience with Cardiologists." At the time of my banning, the thread which began in May 2004, had more than 3150 views, by far the most hits of any thread on the board. I have decided to move my comments about heart disease, hypertension and the lot to Blogspot, where freedom of speech reigns for all, including anyone who would care to reply or comment.
Although I began this blog today, I have back-dated my blood pressure readings to the dates I emailed the reports to my cardiologist. I think many of you with a traditional view of the treatment of hypertension will be surprised.
Although I began this blog today, I have back-dated my blood pressure readings to the dates I emailed the reports to my cardiologist. I think many of you with a traditional view of the treatment of hypertension will be surprised.
Medicate First!!
The American Heart Association and the American College of Cardiologists both state that this condition should be treated with medication FIRST. Why go to the big guns from the get go? I responded very well to meds and my blockages were very very severe (85-100%). And most cardo-thoracic surgeons and invasive cardiologists totally ignore the fact that in people in their 50s, revascularization through angiogenesis picks up the slack left by the coronary vessels that have been compromised. In fact, a CABG usually damages most of the revascularization the body has instituted to heal itself. Why do they do that? Well there's one simple answer, CABGs are much more lucrative than treating this disease with medications.
I have come to believe that if a cardiac physician tells you that you need surgery immediately and you are a walking time bomb waiting to explode or the longer you delay the worse its going to get, you should run, not walk to the nearest board certified noninterventionalist cardiologist and obtain a second opinion. I had been scared into believing the 100% blockages in two of my coronary arteries and 85-90% blockages in the third and other major vessels around my heart meant I would have a heart attack and die at any minute if I didn't have the surgery. Yet, I was told my heart was in good shape. Now what kind of idiot did that interventionalist cardiologist and his cardio-thoracic surgeon buddy think I was? The pipes supplying oxygen to my heart are clogged yet my heart's in good shape? That does not make any sense at all. They didn't tell me about revascularization as the reason my heart was in great shape. Why? because if they did, they knew I would seek another opinion and quite possibly find out my angina was due to hypertension undert physical exertion and they would not get to perform their very expensive lifesaving surgery. As it was, that's exactly what happened. But not because these doctors were ethical and saw that I the patient was fully informed. Oh no, I had to have surgery postponed because the surgeon was not in network with my insurance. Had he been, I would have been one more unnessecary coronary bypass performed in 2004.
I have come to believe that if a cardiac physician tells you that you need surgery immediately and you are a walking time bomb waiting to explode or the longer you delay the worse its going to get, you should run, not walk to the nearest board certified noninterventionalist cardiologist and obtain a second opinion. I had been scared into believing the 100% blockages in two of my coronary arteries and 85-90% blockages in the third and other major vessels around my heart meant I would have a heart attack and die at any minute if I didn't have the surgery. Yet, I was told my heart was in good shape. Now what kind of idiot did that interventionalist cardiologist and his cardio-thoracic surgeon buddy think I was? The pipes supplying oxygen to my heart are clogged yet my heart's in good shape? That does not make any sense at all. They didn't tell me about revascularization as the reason my heart was in great shape. Why? because if they did, they knew I would seek another opinion and quite possibly find out my angina was due to hypertension undert physical exertion and they would not get to perform their very expensive lifesaving surgery. As it was, that's exactly what happened. But not because these doctors were ethical and saw that I the patient was fully informed. Oh no, I had to have surgery postponed because the surgeon was not in network with my insurance. Had he been, I would have been one more unnessecary coronary bypass performed in 2004.
Nine Heart Risk Factors
Nine Heart Risk Factors
------------------------------------------------------------------------
A doctor named Salim Yusuf says there are nine risk factors that account for 90% of all heart attacks. And, we can do something about most of them.
The risk factors include:
* Smoking
* Abnormal cholesterol
* Diabetes
* High blood pressure
* Stress
* Abdominal obesity
* Sedentary lifestyle
* Eating too few fruits and vegetables
* Abstaining from alcohol
A report on CBS News.com's WebMD, says the factors are "equal-opportunity killers," all races, sexes and ages of people can fall victim to these same risks. The study included 30,000 people -- half were first heart attack survivors and half were healthy volunteers of similar ages, races and genders of the heart attack victims.
Generally, they found out
* The bigger the waist, the bigger the risk.
* The bigger the cholesterol particles, the bigger the risk.
* Smoking and a bad lipid ratio accounts for 2/3 of heart disease.
* Smoking alone increases heart attack risk 36%.
* Smoking 3 cigarettes a day wipes out the ptotective effect of aspirin.
* Smoking 3 cigarettes a day wipes out 2/3 of the protective effect of cholesterol lowering drugs.
* Stress doubles the risk of a heart attack.
* A good diet (vegetables & fruit), regular exercise and moderate alcohol intake reduce the risk of heart disease.
Of course diabetes and high blood pressure are factors that are harder to control. However, most people can have their hypertension controlled with medication and diabetes can respond well to weight reduction and dietary changes.
Something I cannot emphasize enough is that many people do not know they have hypertension until it is too late, especially if they are relying on a normal BP finding during physical exams or while getting the BP checked at the pharmacy or supermarket. I always had normal, or even low BP until my cardiologist checked it while I was squeezing a grip testing instrument in my extended right hand for about a minute. My BP shot from 120/70 to 140/110!
I had been having chest tightness (unstable angina) on exertion for months. Little did I realize it was caused by my high blood pressure, even when I would walk as little as four blocks, I would get the chest tightness. My cardiologist put me on Meapropolol, Modiuretic and Monopril starting in June. The anginal pain has disappeared and I am able to do all my normal activities, including mowing my very large yard with a walking mower this morning.
So if you are having angina pain and you don't think you have high blood pressure, ask the doctor to take it while you lay on your back, with your right arm extended in the air squeezing a small rubber ball as hard as you can. You may be very surprised!
------------------------------------------------------------------------
A doctor named Salim Yusuf says there are nine risk factors that account for 90% of all heart attacks. And, we can do something about most of them.
The risk factors include:
* Smoking
* Abnormal cholesterol
* Diabetes
* High blood pressure
* Stress
* Abdominal obesity
* Sedentary lifestyle
* Eating too few fruits and vegetables
* Abstaining from alcohol
A report on CBS News.com's WebMD, says the factors are "equal-opportunity killers," all races, sexes and ages of people can fall victim to these same risks. The study included 30,000 people -- half were first heart attack survivors and half were healthy volunteers of similar ages, races and genders of the heart attack victims.
Generally, they found out
* The bigger the waist, the bigger the risk.
* The bigger the cholesterol particles, the bigger the risk.
* Smoking and a bad lipid ratio accounts for 2/3 of heart disease.
* Smoking alone increases heart attack risk 36%.
* Smoking 3 cigarettes a day wipes out the ptotective effect of aspirin.
* Smoking 3 cigarettes a day wipes out 2/3 of the protective effect of cholesterol lowering drugs.
* Stress doubles the risk of a heart attack.
* A good diet (vegetables & fruit), regular exercise and moderate alcohol intake reduce the risk of heart disease.
Of course diabetes and high blood pressure are factors that are harder to control. However, most people can have their hypertension controlled with medication and diabetes can respond well to weight reduction and dietary changes.
Something I cannot emphasize enough is that many people do not know they have hypertension until it is too late, especially if they are relying on a normal BP finding during physical exams or while getting the BP checked at the pharmacy or supermarket. I always had normal, or even low BP until my cardiologist checked it while I was squeezing a grip testing instrument in my extended right hand for about a minute. My BP shot from 120/70 to 140/110!
I had been having chest tightness (unstable angina) on exertion for months. Little did I realize it was caused by my high blood pressure, even when I would walk as little as four blocks, I would get the chest tightness. My cardiologist put me on Meapropolol, Modiuretic and Monopril starting in June. The anginal pain has disappeared and I am able to do all my normal activities, including mowing my very large yard with a walking mower this morning.
So if you are having angina pain and you don't think you have high blood pressure, ask the doctor to take it while you lay on your back, with your right arm extended in the air squeezing a small rubber ball as hard as you can. You may be very surprised!
Coronary Bypass for a 90-year-old Man!!!
!
boltnut55
Junior Member
Join Date: Jun 2002
Posts: 13
Coronary Bypass for 90 Year Old?
------------------------------------------------------------------------
Hi. My father is almost 90 and two weeks ago was diagnosed w/CHF when he ended up in the ER w/breathing problems. Several days later, he was released (W/O proper meds, which we took care of the next day), but yesterday morning, he ended up in the ER again. This time, the drs. found out he had a small heart attack. Drs. did an angiogram today and found that all three arteries were damaged/clogged (not sure of term). When I asked how much, one dr. said all were 65-90% bad. They didn't do an angioplasty but would have the heart surgeon/team evaluate him over the weekend (he's in a teaching hospital).
Besides cataract/glaucoma and hearing problems, he does have high blood pressure ("normally" 170'ish) and high cholesterol (no idea of numbers). Other than that, he is able to live alone, cook, clean, and bathe... well, until this whole CHF episode, of course.
Is 90 too old to have bypass surgery? I guess I'm trying to figure out if it's automatically a bad idea or whether there should be consideration to his current quality of life, etc. My normal way of handling these situation is to tell him the positive and negative and say, "Dad, you need to decide!" When I explained the angiogram to him, I did tell him there's a chance that they can't do the angioplasty and he might have to have bypass surgery. He said he would agree to the bypass surgery too, but when the drs. told me about the three clogged arteries, one mentioned that the surgical team would still have to evaluate him to see if he's a candidate (as in just cuz dad's willing doesn't mean it'll get done).
If he doesn't get it done, they would do the angioplasty as a backup way and hope it'll take care of the problem. My dad has said that he doesn't need to live to 100. If he can get a few more good years, he'll be happy (always the optimist... not sure why he got me as a pessimistic child!).
Any comments? Answers? HELP!
I just read this very sad thread and what I have to say about this 90-year-old gentleman's physicians would probably be deleted by the moderator. This only serves to reinforce the indictment that some members of the medical community are in it only for the money and to hell with the Hippocratic Oath.
Nine Lives, thanks for reviving this old thread that I had never seen.
boltnut55
Junior Member
Join Date: Jun 2002
Posts: 13
Coronary Bypass for 90 Year Old?
------------------------------------------------------------------------
Hi. My father is almost 90 and two weeks ago was diagnosed w/CHF when he ended up in the ER w/breathing problems. Several days later, he was released (W/O proper meds, which we took care of the next day), but yesterday morning, he ended up in the ER again. This time, the drs. found out he had a small heart attack. Drs. did an angiogram today and found that all three arteries were damaged/clogged (not sure of term). When I asked how much, one dr. said all were 65-90% bad. They didn't do an angioplasty but would have the heart surgeon/team evaluate him over the weekend (he's in a teaching hospital).
Besides cataract/glaucoma and hearing problems, he does have high blood pressure ("normally" 170'ish) and high cholesterol (no idea of numbers). Other than that, he is able to live alone, cook, clean, and bathe... well, until this whole CHF episode, of course.
Is 90 too old to have bypass surgery? I guess I'm trying to figure out if it's automatically a bad idea or whether there should be consideration to his current quality of life, etc. My normal way of handling these situation is to tell him the positive and negative and say, "Dad, you need to decide!" When I explained the angiogram to him, I did tell him there's a chance that they can't do the angioplasty and he might have to have bypass surgery. He said he would agree to the bypass surgery too, but when the drs. told me about the three clogged arteries, one mentioned that the surgical team would still have to evaluate him to see if he's a candidate (as in just cuz dad's willing doesn't mean it'll get done).
If he doesn't get it done, they would do the angioplasty as a backup way and hope it'll take care of the problem. My dad has said that he doesn't need to live to 100. If he can get a few more good years, he'll be happy (always the optimist... not sure why he got me as a pessimistic child!).
Any comments? Answers? HELP!
I just read this very sad thread and what I have to say about this 90-year-old gentleman's physicians would probably be deleted by the moderator. This only serves to reinforce the indictment that some members of the medical community are in it only for the money and to hell with the Hippocratic Oath.
Nine Lives, thanks for reviving this old thread that I had never seen.
RE: Angina
Re: Angina
------------------------------------------------------------------------
Quote:
Originally Posted by alphamale9009
I have slighly elevated blood pressure, but i have angina whether my blood pressure is high or not. Atenolol has worked, but only at a dosage of 200mg a day. I want to get off the Atenolol because it lowers testosterone, and perhaps there is something that works better. Has anyone used a medication that has gotten rid of heart pain? What was it, was there any side effects? Any responses will be appreciated.
alpha
Alpha,
I am just starting week two of my medical program. I have been completely assymptomatic since beginning it.
Here is my medication regimen:
Week One - Metoprolol 50mg bid; Moduretic (amiloride/hydrochlorothiazide 5/50mg 1 tablet q am
Week Three - Increase Metoprolol to 75mg bid;
Week Five - Increase Moduretic to 2 tablets q am; Keep Metoprolol the same.
Week Seven - Fosinopril 10mg at bedtime; all other meds as before.
Week Nine - Increase Fosinopril to 15mg hs; all other meds stay the same.
Week Eleven - Increase Fosinopril to 20 mg hs; all other meds stay the same.
Week Twelve - Depending on my blood pressure readings, adding Isordil three times a day at an incremental rate of 1, 1 1/2, and 2 tablets every eight hours or 1/2, 1, and 1 1/2 tablets q8h; all other meds stay the same.
BTW, my primary care physician had me on atenolol for about three weeks before I started this program. It made me practically impotent. I am okay sexually on these meds.
------------------------------------------------------------------------
Quote:
Originally Posted by alphamale9009
I have slighly elevated blood pressure, but i have angina whether my blood pressure is high or not. Atenolol has worked, but only at a dosage of 200mg a day. I want to get off the Atenolol because it lowers testosterone, and perhaps there is something that works better. Has anyone used a medication that has gotten rid of heart pain? What was it, was there any side effects? Any responses will be appreciated.
alpha
Alpha,
I am just starting week two of my medical program. I have been completely assymptomatic since beginning it.
Here is my medication regimen:
Week One - Metoprolol 50mg bid; Moduretic (amiloride/hydrochlorothiazide 5/50mg 1 tablet q am
Week Three - Increase Metoprolol to 75mg bid;
Week Five - Increase Moduretic to 2 tablets q am; Keep Metoprolol the same.
Week Seven - Fosinopril 10mg at bedtime; all other meds as before.
Week Nine - Increase Fosinopril to 15mg hs; all other meds stay the same.
Week Eleven - Increase Fosinopril to 20 mg hs; all other meds stay the same.
Week Twelve - Depending on my blood pressure readings, adding Isordil three times a day at an incremental rate of 1, 1 1/2, and 2 tablets every eight hours or 1/2, 1, and 1 1/2 tablets q8h; all other meds stay the same.
BTW, my primary care physician had me on atenolol for about three weeks before I started this program. It made me practically impotent. I am okay sexually on these meds.
Collateral Circulation
Collateral Circulation
------------------------------------------------------------------------
I thought I'd try to begin a thread on the very important issue of collateral circulation as it realated to cardiac survival.
It's a remarkable process where myriad routes of tiny arterioles and capillaries expand in size and number to carry blood around an arterial blockage (and presumbably in venous blockage also!)
The collateral circulation can be from the top of a blockage (proximal) to a point beyond the blockage at the bottom (distal) thus mititgating the effect of an otherwise damaging and often deadly cessation of blood flow.
Amazingly sometimes the routing is even from one artery to another often spanning accross the heart from the left decending system to the circumflex or even RCA (right) system.
Obviously the blockage spurs the circulation and it becomes a race to see if the collateralization keeps up or a heart attack occurs!
I survived for at least a decade with collaterals around a virtually complete RCA blockage from top proximal to distal right artery (same one.) I only noticed the deficiency of blood flow during peak stress....maybe 5-10 minutes a day max!
Now, HOW do we make the collateralization progress faster than the blocking? Neither drug companies nor cardiologists really seem to care about the topic (quite naturally- we live in a capitalist society.)
But WE MUST care! We MUST find a way to enhance this process.
Let me throw a couple of my thoughts out ("Partially baked ideas", if you will: an old Mensa term for decent thoughts not fleshed out...NEVER to be confused with HALF baked ideas )
I'm an engineer and I know that hydraulics demonstrates that a way to push a new channel through is higher pressure. Is perhaps high blood pressure a way that evolution has blessed mankind in its need for coronary and cerebral collaterals...not likely that the everpresent hypertension developed from cave man days solely to enrich doctors and drug manufacturers...or to give us red faces when we get angry!
This line of thinking also goes to the subject of hard cardiac workouts to get BP up so high that it can safely force through some new arteries when needed (without blowing any out )...I'm thinking Ubernier's peak exercising (and mine lately as well )
It has always struck me a wrong-thinking to use drugs that weaken the heart's pumping ability and strength (beta and calcium channel blockers) in an effort to develop cardiac health. Lessening of pain frequency may be admirable but what if it's at the cost of slowing down auto-revascularization.
Perhaps all the studies that show that people with high blood pressure are at higher risk of heart disease have it asp backwards. Maybe the growing blockages are putting the body into a state where it it most able to revascularize with higher hydraulic pressure to force new channels! If this is correct then perhaps ALL methods of BP overcontrol are counterproductive for cardiac health, fighting the body's best efforts to survive!
Of course, it would seem any method to stop clotting (such as daily aspirin) which will prevent catastrophic total blockage, or any any anti inflammatories (also aspirin) which will prevent plaques from becoming unstable and blowing open...also causing clotting and blocking are HIGHLY desirable to buy time for the slow coollateraliztion.
I've seen some research last week on drugs that hope to stop cancer's ability to "call" vascularization from adjoining vessels, a process which allows the tumor to feed. These drugs might be effective at blocking certain receptors on blood vessels so they don't grow over to the nearby tumor, thus starving it.
Maybe we should be learning from the cancer cell and develop some of it's chemical devices to SPUR vascularization where needed...perhaps in people with 40% blockages, or some arbitrary break even point between benefit and risk.
Any thoughts?
------------------------------------------------------------------------
Last edited by zip2play : 06-17-2004 at 03:52 PM.
zip2play
View Public Profile
Find all posts by zip2play
Add zip2play to Your Buddy List
Sponsored Links
#2
06-17-2004, 04:57 PM
wordworks2001
Banned
Join Date: May 2004
Posts: 133
Re: Collateral Circulation
------------------------------------------------------------------------
There are two sources I found when I was researching noninvasive alternatives to treatment for CAD. One is from the journal Circulation. 2002;105:666 and the other is from Reviews in Cardiovascular Medicine 2002;3:5.
The Veterans Affairs Non-Q-Wave Infarctions Strategies in Hospital (VANQWISH) trial showed the noninvasive strategies not only to be more economical, but those who were treated medically had better survival 76% of the time.
This is one of the more recent studies I cited to Dr. Wayne's detractors on this board and that no one was able to effectively refute. But that is an old discussion from another flood.
Thanks for renewing the debate Zip2play. I will review what is written here faithfully and perhaps even contribute now and then. However, I am far from a candidate for MENSA, so I will probably be more of an observer.
Jeff
------------------------------------------------------------------------
I thought I'd try to begin a thread on the very important issue of collateral circulation as it realated to cardiac survival.
It's a remarkable process where myriad routes of tiny arterioles and capillaries expand in size and number to carry blood around an arterial blockage (and presumbably in venous blockage also!)
The collateral circulation can be from the top of a blockage (proximal) to a point beyond the blockage at the bottom (distal) thus mititgating the effect of an otherwise damaging and often deadly cessation of blood flow.
Amazingly sometimes the routing is even from one artery to another often spanning accross the heart from the left decending system to the circumflex or even RCA (right) system.
Obviously the blockage spurs the circulation and it becomes a race to see if the collateralization keeps up or a heart attack occurs!
I survived for at least a decade with collaterals around a virtually complete RCA blockage from top proximal to distal right artery (same one.) I only noticed the deficiency of blood flow during peak stress....maybe 5-10 minutes a day max!
Now, HOW do we make the collateralization progress faster than the blocking? Neither drug companies nor cardiologists really seem to care about the topic (quite naturally- we live in a capitalist society.)
But WE MUST care! We MUST find a way to enhance this process.
Let me throw a couple of my thoughts out ("Partially baked ideas", if you will: an old Mensa term for decent thoughts not fleshed out...NEVER to be confused with HALF baked ideas )
I'm an engineer and I know that hydraulics demonstrates that a way to push a new channel through is higher pressure. Is perhaps high blood pressure a way that evolution has blessed mankind in its need for coronary and cerebral collaterals...not likely that the everpresent hypertension developed from cave man days solely to enrich doctors and drug manufacturers...or to give us red faces when we get angry!
This line of thinking also goes to the subject of hard cardiac workouts to get BP up so high that it can safely force through some new arteries when needed (without blowing any out )...I'm thinking Ubernier's peak exercising (and mine lately as well )
It has always struck me a wrong-thinking to use drugs that weaken the heart's pumping ability and strength (beta and calcium channel blockers) in an effort to develop cardiac health. Lessening of pain frequency may be admirable but what if it's at the cost of slowing down auto-revascularization.
Perhaps all the studies that show that people with high blood pressure are at higher risk of heart disease have it asp backwards. Maybe the growing blockages are putting the body into a state where it it most able to revascularize with higher hydraulic pressure to force new channels! If this is correct then perhaps ALL methods of BP overcontrol are counterproductive for cardiac health, fighting the body's best efforts to survive!
Of course, it would seem any method to stop clotting (such as daily aspirin) which will prevent catastrophic total blockage, or any any anti inflammatories (also aspirin) which will prevent plaques from becoming unstable and blowing open...also causing clotting and blocking are HIGHLY desirable to buy time for the slow coollateraliztion.
I've seen some research last week on drugs that hope to stop cancer's ability to "call" vascularization from adjoining vessels, a process which allows the tumor to feed. These drugs might be effective at blocking certain receptors on blood vessels so they don't grow over to the nearby tumor, thus starving it.
Maybe we should be learning from the cancer cell and develop some of it's chemical devices to SPUR vascularization where needed...perhaps in people with 40% blockages, or some arbitrary break even point between benefit and risk.
Any thoughts?
------------------------------------------------------------------------
Last edited by zip2play : 06-17-2004 at 03:52 PM.
zip2play
View Public Profile
Find all posts by zip2play
Add zip2play to Your Buddy List
Sponsored Links
#2
06-17-2004, 04:57 PM
wordworks2001
Banned
Join Date: May 2004
Posts: 133
Re: Collateral Circulation
------------------------------------------------------------------------
There are two sources I found when I was researching noninvasive alternatives to treatment for CAD. One is from the journal Circulation. 2002;105:666 and the other is from Reviews in Cardiovascular Medicine 2002;3:5.
The Veterans Affairs Non-Q-Wave Infarctions Strategies in Hospital (VANQWISH) trial showed the noninvasive strategies not only to be more economical, but those who were treated medically had better survival 76% of the time.
This is one of the more recent studies I cited to Dr. Wayne's detractors on this board and that no one was able to effectively refute. But that is an old discussion from another flood.
Thanks for renewing the debate Zip2play. I will review what is written here faithfully and perhaps even contribute now and then. However, I am far from a candidate for MENSA, so I will probably be more of an observer.
Jeff
RE: Two Basic Angina Questions
Re: 2 basic angina questions
------------------------------------------------------------------------
Quote:
Originally Posted by EWF
Hi, there ... I hope someone can clear up 2 questions (mostly out of curiousity) that have been floating around in my mind lately:
1. It is said that most exercise-induced angina lasts only a few minutes and then subsides when activity is stopped. So I'm curious, if one does not stop exercising upon feeling the pain, wouldn't the pain then last for the entire duration of the activity, i.e., more than just a few minutes?
2. Is angina always accompanied by shortness of breath?
Thanks for any insights anyone may have to offer.
I can only speak to my angina symptoms. Before I began treatment, I would get a tightness in my chest that would last for about five minutes after I ceased the activity that precipitated the discomfort. I would not characterize the sensation as "pain." It usually was not accompanied by shortness of breath but I do recall one instance when I was walking up a long hill when it was. I sometimes didn't stop and wait for the discomfort to subside and it never got worse once it reached a certain point. So to answer your question -- Yes. I was given NTG 4mg to take sublingually three times five minutes apart. Often it would not stop the symptoms, only rest would.
My chest tightness could be caused by walking briskly a few blocks or carrying heavy objects. I have not had the chest tightness since I began my medical program.
------------------------------------------------------------------------
Quote:
Originally Posted by EWF
Hi, there ... I hope someone can clear up 2 questions (mostly out of curiousity) that have been floating around in my mind lately:
1. It is said that most exercise-induced angina lasts only a few minutes and then subsides when activity is stopped. So I'm curious, if one does not stop exercising upon feeling the pain, wouldn't the pain then last for the entire duration of the activity, i.e., more than just a few minutes?
2. Is angina always accompanied by shortness of breath?
Thanks for any insights anyone may have to offer.
I can only speak to my angina symptoms. Before I began treatment, I would get a tightness in my chest that would last for about five minutes after I ceased the activity that precipitated the discomfort. I would not characterize the sensation as "pain." It usually was not accompanied by shortness of breath but I do recall one instance when I was walking up a long hill when it was. I sometimes didn't stop and wait for the discomfort to subside and it never got worse once it reached a certain point. So to answer your question -- Yes. I was given NTG 4mg to take sublingually three times five minutes apart. Often it would not stop the symptoms, only rest would.
My chest tightness could be caused by walking briskly a few blocks or carrying heavy objects. I have not had the chest tightness since I began my medical program.
A Reply to a Cardiologist
wordworks2001
Banned
Join Date: May 2004
Posts: 133
Test5629
------------------------------------------------------------------------
At the risk of insulting you more, remember what I said about Dr. Wayne spending 5 UNINTERUPTED hours with me? Check out this article from the New York Times.
Michael J. Okoniewski for The New York Times
Tell the Doctor All Your Problems, but Keep It to Less Than a Minute
By MEREDITH LEVINE
Published: June 1, 2004
woman walks into a doctor's office. The doctor says, "What brings you here today?" The woman starts to answer. Eighteen seconds later, the doctor interrupts.
This may sound like the setup to a lame joke but it is a scene played out regularly in doctors' offices across the country. Two decades ago, in 1984, researchers showed that on average, patients were interrupted 18 seconds into explaining their problems. Fewer than 2 percent got to finish their explanations.
Advertisement
But at the time, the office or bedside manner of doctors was considered unworthy of research.
"We were thought of as weirdos," said Dr. Howard Beckman, co-author of the study and a clinical professor of medicine at the University of Rochester.
Today, however, the rise of managed care has helped make doctor-patient communication a major issue that is drawing increasing interest from researchers.
Researchers have linked poor communication to misdiagnoses, the ordering of unnecessary tests, and the failure of patients to follow treatment plans.
"When communication doesn't work and patients have good outcomes, it's by chance," said Dr. Sherrie H. Kaplan, an associate dean in the college of medicine at the University of California, Irvine, and a leading researcher in the field.
Just how often does communication between doctors and patients run amok? Research shows that only 15 percent of patients fully understand what their doctors tell them, and that 50 percent leave their doctors' offices uncertain of what they are supposed to do to take care of themselves. Studies suggest that women are better at building relationships with their doctors than men. The typical number of questions a male patient asks during a 15-minute doctor's visit is zero, while women average six, according to a study by Dr. Kaplan.
Doctors as well as patients may suffer the consequences of communication gone awry. A common theme of malpractice lawsuits is a breakdown in communication, said Dr. Wendy Levinson, vice chairwoman of the University of Toronto's department of medicine. What often prompts people to sue their doctors, said Dr. Levinson, who has studied the issue extensively, "is the feeling that they were not listened to, that they didn't have the doctor's full attention."
In one study, Dr. Levinson and Dr. Nalini Ambady, a psychologist at Harvard, compared the office manner of surgeons who had been sued multiple times with those who had never been sued. Doctors with "a more dominant tone of voice," they found, were more likely to have been sued by patients. Doctors whose voices contained more warmth were less likely to have been sued.
In many instances, the lawsuits have little to do with physical harm to the patient, the researchers said, and much to do with the relationship between doctor and patient. Patients who sue often feel abandoned by their doctors.
Advice by experts on how doctors can most effectively communicate with patients reads as if it came straight out of a relationship self-help book: Listen carefully, ask open-ended questions, do not interrupt, make eye contact and indicate that you care.
Good doctors, communication experts say, do not pepper patients with questions; patients, studies find, do not like that.
A doctor's medical competence is of course important. And patients sometimes stick with doctors they feel are cold or uncommunicative in the belief that a physician's technical and diagnostic skills are more important than bedside manner. But, Dr. Levinson said, competence and communication are equally important.
"We should consider excellence a combination of the most technically sophisticated skills and knowledge and the best communication skills," she said, "because that will get us the best outcomes from our patients."
Research has shown that there is a clear connection between positive doctor-patient relationships and improvements in the patients' health.
In several studies, Dr. Kaplan and her husband, Dr. Sheldon Greenfield, also of the University of California at Irvine, found that good doctor-patient communication resulted in lower blood sugar levels in diabetic patients, and lower blood pressure in hypertensive patients.
Banned
Join Date: May 2004
Posts: 133
Test5629
------------------------------------------------------------------------
At the risk of insulting you more, remember what I said about Dr. Wayne spending 5 UNINTERUPTED hours with me? Check out this article from the New York Times.
Michael J. Okoniewski for The New York Times
Tell the Doctor All Your Problems, but Keep It to Less Than a Minute
By MEREDITH LEVINE
Published: June 1, 2004
woman walks into a doctor's office. The doctor says, "What brings you here today?" The woman starts to answer. Eighteen seconds later, the doctor interrupts.
This may sound like the setup to a lame joke but it is a scene played out regularly in doctors' offices across the country. Two decades ago, in 1984, researchers showed that on average, patients were interrupted 18 seconds into explaining their problems. Fewer than 2 percent got to finish their explanations.
Advertisement
But at the time, the office or bedside manner of doctors was considered unworthy of research.
"We were thought of as weirdos," said Dr. Howard Beckman, co-author of the study and a clinical professor of medicine at the University of Rochester.
Today, however, the rise of managed care has helped make doctor-patient communication a major issue that is drawing increasing interest from researchers.
Researchers have linked poor communication to misdiagnoses, the ordering of unnecessary tests, and the failure of patients to follow treatment plans.
"When communication doesn't work and patients have good outcomes, it's by chance," said Dr. Sherrie H. Kaplan, an associate dean in the college of medicine at the University of California, Irvine, and a leading researcher in the field.
Just how often does communication between doctors and patients run amok? Research shows that only 15 percent of patients fully understand what their doctors tell them, and that 50 percent leave their doctors' offices uncertain of what they are supposed to do to take care of themselves. Studies suggest that women are better at building relationships with their doctors than men. The typical number of questions a male patient asks during a 15-minute doctor's visit is zero, while women average six, according to a study by Dr. Kaplan.
Doctors as well as patients may suffer the consequences of communication gone awry. A common theme of malpractice lawsuits is a breakdown in communication, said Dr. Wendy Levinson, vice chairwoman of the University of Toronto's department of medicine. What often prompts people to sue their doctors, said Dr. Levinson, who has studied the issue extensively, "is the feeling that they were not listened to, that they didn't have the doctor's full attention."
In one study, Dr. Levinson and Dr. Nalini Ambady, a psychologist at Harvard, compared the office manner of surgeons who had been sued multiple times with those who had never been sued. Doctors with "a more dominant tone of voice," they found, were more likely to have been sued by patients. Doctors whose voices contained more warmth were less likely to have been sued.
In many instances, the lawsuits have little to do with physical harm to the patient, the researchers said, and much to do with the relationship between doctor and patient. Patients who sue often feel abandoned by their doctors.
Advice by experts on how doctors can most effectively communicate with patients reads as if it came straight out of a relationship self-help book: Listen carefully, ask open-ended questions, do not interrupt, make eye contact and indicate that you care.
Good doctors, communication experts say, do not pepper patients with questions; patients, studies find, do not like that.
A doctor's medical competence is of course important. And patients sometimes stick with doctors they feel are cold or uncommunicative in the belief that a physician's technical and diagnostic skills are more important than bedside manner. But, Dr. Levinson said, competence and communication are equally important.
"We should consider excellence a combination of the most technically sophisticated skills and knowledge and the best communication skills," she said, "because that will get us the best outcomes from our patients."
Research has shown that there is a clear connection between positive doctor-patient relationships and improvements in the patients' health.
In several studies, Dr. Kaplan and her husband, Dr. Sheldon Greenfield, also of the University of California at Irvine, found that good doctor-patient communication resulted in lower blood sugar levels in diabetic patients, and lower blood pressure in hypertensive patients.
The State of Our Health Care Delivery System
Here is another interesting article about the state of our health care delivery system:
Study Finds Widespread Problem of Inadequate Health Care
By LAWRENCE K. ALTMAN (NYT) 753 words
Americans get substandard care for their ailments about half the time, even if they live near a major teaching hospital, the first comprehensive study of health care provided in metropolitan areas has found.
The inadequate treatment leads to ''thousands of needless deaths each year,'' said Dr. Elizabeth A. McGlynn, a researcher at the RAND Corporation and an author of the study, being published today in the journal Health Affairs.
Only a fundamental redesign of the health system will improve the situation, Dr. McGlynn said, adding, ''It's a tremendous cultural shift we're asking for.''
The study's conclusions were based chiefly on a review of the medical records of nearly 7,000 people in 12 metropolitan areas, including Newark, Miami and Orange County, Calif. On average, the authors found, patients received substandard care, as defined by leading medical groups, 50 percent to 60 percent of the time. There was little variation among the metropolitan areas, randomly selected from 60 with populations of at least 200,000. The areas included cities and their suburbs.
Dr. McGlynn said the study's definitions of adequate care were developed not only from the recommendations published by specialty medical groups but also from four panels of doctors who practiced in a variety of settings. The recommendations reflected what was considered standard at the time the care in the study was delivered, from 1996 to 2000.
The team used the standards to measure average care for adults in an entire community, not the care delivered by specific hospitals, health care plans or doctors. The study did not make comparisons with earlier years or other countries.
''Quality in most areas of care was uniformly poor,'' said the authors of the study, which was financed by the Robert Wood Johnson Foundation. And Dr. McGlynn added that for the $1.4 trillion a year the United States spends on health care, it was getting ''fairly dismal results.''
In a telephone interview with reporters, she noted that doctors and hospitals were paid the same whether they provided ''very good care or not-so-good care.''
Dr. Donald J. Palmisano, president of the American Medical Association, said yesterday that ''there is room for improvement'' in medical care and that his organization had taken steps so that new recommendations and innovations are quickly communicated to all physicians.
''The main challenge is quick retrieval of pertinent information,'' Dr. Palmisano said in an interview from a meeting on improving patient safety he was attending in Boston.
Although other researchers have concluded that American health care falls far short of its potential, their studies have not been as broadly based as the new one.
To assess the level of care in the 12 communities, the authors received permission from the patients who participated to scour their medical records for the two preceding years. The authors recorded information concerning 439 steps involved in the care of 30 acute and chronic medical conditions like high blood pressure, immunizations, heart failure, diabetes, broken hips and alcoholism.
For diabetes, the steps included measurements of blood pressure, blood sugar, cholesterol and examination of the feet and eyes. The steps were intended to measure control of the disease and its complications.
Quality of care for some chronic diseases was variable. High blood pressure ranked among the best while diabetes care ranked lowest in most communities, the authors said. Preventive care for sexually transmitted diseases, AIDS and substance abuse ranked lower than screening for high blood pressure and offering immunizations.
Saying that information about quality should be presented locally so officials could tailor action to community needs, the authors urged greater collaboration among communities to improve monitoring of health care.
As models, the authors cited efforts that 43 medical groups and hospitals in Minnesota were making to develop uniform practice guidelines for all health plans in the state. The authors also said monitoring and public reporting of heart bypass surgery in New York State had led to a decline in deaths from the procedure.
The authors also called on research agencies to conduct studies involving larger numbers of communities. They said it would require a study of more than 100 metropolitan areas to draw more definitive conclusions about the effects of the structure of health care systems and finances. (Besides Newark, Miami and Orange County, the areas studied were Boston; Cleveland; Greenville, S.C.; Indianapolis; Lansing, Mich.; Little Rock, Ark.; Phoenix; Seattle; and Syracuse.)
Study Finds Widespread Problem of Inadequate Health Care
By LAWRENCE K. ALTMAN (NYT) 753 words
Americans get substandard care for their ailments about half the time, even if they live near a major teaching hospital, the first comprehensive study of health care provided in metropolitan areas has found.
The inadequate treatment leads to ''thousands of needless deaths each year,'' said Dr. Elizabeth A. McGlynn, a researcher at the RAND Corporation and an author of the study, being published today in the journal Health Affairs.
Only a fundamental redesign of the health system will improve the situation, Dr. McGlynn said, adding, ''It's a tremendous cultural shift we're asking for.''
The study's conclusions were based chiefly on a review of the medical records of nearly 7,000 people in 12 metropolitan areas, including Newark, Miami and Orange County, Calif. On average, the authors found, patients received substandard care, as defined by leading medical groups, 50 percent to 60 percent of the time. There was little variation among the metropolitan areas, randomly selected from 60 with populations of at least 200,000. The areas included cities and their suburbs.
Dr. McGlynn said the study's definitions of adequate care were developed not only from the recommendations published by specialty medical groups but also from four panels of doctors who practiced in a variety of settings. The recommendations reflected what was considered standard at the time the care in the study was delivered, from 1996 to 2000.
The team used the standards to measure average care for adults in an entire community, not the care delivered by specific hospitals, health care plans or doctors. The study did not make comparisons with earlier years or other countries.
''Quality in most areas of care was uniformly poor,'' said the authors of the study, which was financed by the Robert Wood Johnson Foundation. And Dr. McGlynn added that for the $1.4 trillion a year the United States spends on health care, it was getting ''fairly dismal results.''
In a telephone interview with reporters, she noted that doctors and hospitals were paid the same whether they provided ''very good care or not-so-good care.''
Dr. Donald J. Palmisano, president of the American Medical Association, said yesterday that ''there is room for improvement'' in medical care and that his organization had taken steps so that new recommendations and innovations are quickly communicated to all physicians.
''The main challenge is quick retrieval of pertinent information,'' Dr. Palmisano said in an interview from a meeting on improving patient safety he was attending in Boston.
Although other researchers have concluded that American health care falls far short of its potential, their studies have not been as broadly based as the new one.
To assess the level of care in the 12 communities, the authors received permission from the patients who participated to scour their medical records for the two preceding years. The authors recorded information concerning 439 steps involved in the care of 30 acute and chronic medical conditions like high blood pressure, immunizations, heart failure, diabetes, broken hips and alcoholism.
For diabetes, the steps included measurements of blood pressure, blood sugar, cholesterol and examination of the feet and eyes. The steps were intended to measure control of the disease and its complications.
Quality of care for some chronic diseases was variable. High blood pressure ranked among the best while diabetes care ranked lowest in most communities, the authors said. Preventive care for sexually transmitted diseases, AIDS and substance abuse ranked lower than screening for high blood pressure and offering immunizations.
Saying that information about quality should be presented locally so officials could tailor action to community needs, the authors urged greater collaboration among communities to improve monitoring of health care.
As models, the authors cited efforts that 43 medical groups and hospitals in Minnesota were making to develop uniform practice guidelines for all health plans in the state. The authors also said monitoring and public reporting of heart bypass surgery in New York State had led to a decline in deaths from the procedure.
The authors also called on research agencies to conduct studies involving larger numbers of communities. They said it would require a study of more than 100 metropolitan areas to draw more definitive conclusions about the effects of the structure of health care systems and finances. (Besides Newark, Miami and Orange County, the areas studied were Boston; Cleveland; Greenville, S.C.; Indianapolis; Lansing, Mich.; Little Rock, Ark.; Phoenix; Seattle; and Syracuse.)
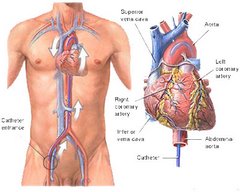
Is a Heart Cath Really Necessary?
Re: Is a Heart Cath really necessary???
------------------------------------------------------------------------
Quote:
Originally Posted by KShortie
Hi there. I had a heart catheterization, and it truly is the only test that gives the doctors the entire picture of whether there is blockage in your heart or not. It is invasive, but only a catheter is threaded up through the vein in your groin so it isn't like surgery. It's actually quite fast, I don't think it took over fifteen to twenty minutes once there in there looking. It really wasn't painful either. So if you are worried go ahead and have it.
Good luck!
Dr. Howard Wayne, pioneer in noninvasive diagnosis and treatment of heart disease said in his book, Living Longer with Heart Disease:
"The Holy Grail for cardiologists is the angiogram. It is worshipped with a religious fervor unlike any test in medicine. Go to any invasive or interventionalist cardiologist and he or she will invariably recommend an angiogram either the same day or the next day -- and will often become upset if you refuse...
"Is the cardiologist's faith in this procedure justified? Is the information the angiogram provides reliable? Can it tell the doctor how his or her patients should be treated, and if they are likely to have a heart attack and die? Will it provide information that can't be obtained in any other way? And, most importantly, is it even necessary to know whether and where an artery is narrowed to treat the patient? In simple terms, is the angiogram recommended for the patient's -- or for the doctor's benefit?...
"...When coronary artery disease is found on an angiogram, the cardiologist cannot be sure whether it is causing the patient's symptoms, or if the disease has been present for years...
"...there is very poor correlation between the anatomical amount of coronary artery disease and the presence or absence of symptoms..."
Bottom line regarding angiograms:
They cannot determine the cause of chest pain.
They cannot predict a heart attack.
Finally, Dr. Wayne, Fellow of the American College of Cardiology and American College of Physicians, has said "It cannot be emphasized strongly enough that the cornary angiogram is one of the most inaccurate and unreliable tests in all of cardiology. More often than not it leads to the wrong diagnosis, and results in inapprpriate and unnecessary treatment. It has little relationship to symptoms, it does not relate to the cause of the patient's symptoms, it correlates poorly with the function of the heart, and it cannot accurately predict the occurence of a heart attack. Immediate angiograms are done solely for economic reasons, not medical reasons. "
------------------------------------------------------------------------
Quote:
Originally Posted by KShortie
Hi there. I had a heart catheterization, and it truly is the only test that gives the doctors the entire picture of whether there is blockage in your heart or not. It is invasive, but only a catheter is threaded up through the vein in your groin so it isn't like surgery. It's actually quite fast, I don't think it took over fifteen to twenty minutes once there in there looking. It really wasn't painful either. So if you are worried go ahead and have it.
Good luck!
Dr. Howard Wayne, pioneer in noninvasive diagnosis and treatment of heart disease said in his book, Living Longer with Heart Disease:
"The Holy Grail for cardiologists is the angiogram. It is worshipped with a religious fervor unlike any test in medicine. Go to any invasive or interventionalist cardiologist and he or she will invariably recommend an angiogram either the same day or the next day -- and will often become upset if you refuse...
"Is the cardiologist's faith in this procedure justified? Is the information the angiogram provides reliable? Can it tell the doctor how his or her patients should be treated, and if they are likely to have a heart attack and die? Will it provide information that can't be obtained in any other way? And, most importantly, is it even necessary to know whether and where an artery is narrowed to treat the patient? In simple terms, is the angiogram recommended for the patient's -- or for the doctor's benefit?...
"...When coronary artery disease is found on an angiogram, the cardiologist cannot be sure whether it is causing the patient's symptoms, or if the disease has been present for years...
"...there is very poor correlation between the anatomical amount of coronary artery disease and the presence or absence of symptoms..."
Bottom line regarding angiograms:
They cannot determine the cause of chest pain.
They cannot predict a heart attack.
Finally, Dr. Wayne, Fellow of the American College of Cardiology and American College of Physicians, has said "It cannot be emphasized strongly enough that the cornary angiogram is one of the most inaccurate and unreliable tests in all of cardiology. More often than not it leads to the wrong diagnosis, and results in inapprpriate and unnecessary treatment. It has little relationship to symptoms, it does not relate to the cause of the patient's symptoms, it correlates poorly with the function of the heart, and it cannot accurately predict the occurence of a heart attack. Immediate angiograms are done solely for economic reasons, not medical reasons. "
Noninvasive Diagnosis of CAD
Noninvasive Diagnosis of CAD
------------------------------------------------------------------------
It seems I have started a debate on Noninvasive Treatment of CAD. Now let me take this subject one step further by discussing noninvasive diagnosis of CAD.
Dr. Howard Wayne of the Noninvasive Heart Center of San Diego says "Noninvasive testing entails placing radioactive detectors, sonar devices, pulse transducers and microphones on the chest. No catheters, tubes or needles enter or "invade" the body.
Non invasive tests and images permanently record:
* localized abnormalities of motion of heart muscle due to obstructive coronary artery disease.
* flow of blood in heart muscle.
* thickness of heart muscle walls.
* dimensions of heart's chambers.
* structure and motion of its valves.
* obstruction or leakage of valves.
* heart murmurs: their origin and the volume, velocity and pattern of blood flow through each valve.
* duration of each phase of the cardiac cycle (electrical activation, rise in pressure, ejection of blood, relaxation, early and late filling of the heart, and atrial contraction).
* normal and abnormal heart sounds.
* systolic and diastolic heart function.
* fraction of blood ejected each beat.
Heart disease, if present, will be found with resting, noninvasive tests in 85-90% of patients. Even those without symptoms. Exercise tests with noninvasive studies will identify almost all of the remainder.
Lest the readers of this post think this is the insane ramblings of a "quack," I reiterate Dr. Wayne's credentials: He is a fellow of the American College of Cardiology and American College of Physicians.
His belief in noninvasive diagnostic and treatment techniques are also endorsed by these two independent websites:
[url]www.physsportmed.com/issues/2000/01_00/roos.htm[/url]
[url]www.hearts.sutterhealth.org/health/conditions/cad.html[/url]
You will note this site not only lists noninvasive diagnostic techniques, it lists coronary bypass surgery as a last resort.
------------------------------------------------------------------------
It seems I have started a debate on Noninvasive Treatment of CAD. Now let me take this subject one step further by discussing noninvasive diagnosis of CAD.
Dr. Howard Wayne of the Noninvasive Heart Center of San Diego says "Noninvasive testing entails placing radioactive detectors, sonar devices, pulse transducers and microphones on the chest. No catheters, tubes or needles enter or "invade" the body.
Non invasive tests and images permanently record:
* localized abnormalities of motion of heart muscle due to obstructive coronary artery disease.
* flow of blood in heart muscle.
* thickness of heart muscle walls.
* dimensions of heart's chambers.
* structure and motion of its valves.
* obstruction or leakage of valves.
* heart murmurs: their origin and the volume, velocity and pattern of blood flow through each valve.
* duration of each phase of the cardiac cycle (electrical activation, rise in pressure, ejection of blood, relaxation, early and late filling of the heart, and atrial contraction).
* normal and abnormal heart sounds.
* systolic and diastolic heart function.
* fraction of blood ejected each beat.
Heart disease, if present, will be found with resting, noninvasive tests in 85-90% of patients. Even those without symptoms. Exercise tests with noninvasive studies will identify almost all of the remainder.
Lest the readers of this post think this is the insane ramblings of a "quack," I reiterate Dr. Wayne's credentials: He is a fellow of the American College of Cardiology and American College of Physicians.
His belief in noninvasive diagnostic and treatment techniques are also endorsed by these two independent websites:
[url]www.physsportmed.com/issues/2000/01_00/roos.htm[/url]
[url]www.hearts.sutterhealth.org/health/conditions/cad.html[/url]
You will note this site not only lists noninvasive diagnostic techniques, it lists coronary bypass surgery as a last resort.
Bill Clinton Should Have My Health Insurance
It’s too bad that former President Bill Clinton didn’t have the same insurance company I had. If he did, he might have been spared a great deal of pain and surgery-induced heartache. He also might have extended his life and saved some money in the process.
Like Clinton, I began to experience chest tightness earlier this year. Ironically, it happened whenever I did the one thing we’re always told we don’t do enough of: exercise. I’d walk only a few blocks, and I’d feel a non-painful chest tightness and shortness of breath. It went away when I was at rest.
In April, my primary care physician performed an EKG that appeared normal. Even so, she felt that I should consult a cardiologist and seek further tests. The cardiologist at the state-of-the-art, multi-million dollar Indiana Heart Hospital ordered a stress test and imaging study of my heart, the results of which were deemed “abnormal.”
The cardiologist scheduled me for an angiogram, an invasive procedure in which a catheter with a camera on the end is inserted in the leg and threaded into the heart to get a closer look. I was warned that I likely had blockages in one or more coronary arteries that would require the placement of stents.
The doctor’s reaction when I requested the procedure to be postponed until May because of a planned vacation led me to believe that my situation was not life-threatening.
At 5:30 a.m. on May 10, I arrived at the four-star hotel they call the Indiana Heart Hospital for the outpatient procedure. A guest relations representative escorted me through the double doors to a small room in Suite C.
As I emerged from my twilight sleep, I was double-teamed by my heart specialist and a cardiothoracic surgeon he had paged for an emergency consult. The specialist told me that I had massive blockages to each of my three coronary arteries and surrounding vessels that supply oxygen to my heart. He said so many blockages were involved that stents would not be effective. I would need a quintuple bypass.
The surgeon, summoning up his most understanding bedside manner, shared that he understood how I felt because he had undergone surgery recently himself. It was Monday, and he anticipated doing the surgery on Wednesday or Thursday. The surgeon explained that I would need pre-operative instruction, which would be best for me to do while still in the hospital.
On Wednesday night, I prepared for Thursday morning surgery just as the physical therapist and nurse had instructed. But that same nurse called and said that the surgeon was not in network with my insurance. The procedure would be postponed until a network surgeon could be found.
A retired Army nurse, I normally would be the first to conduct in-depth research into any diagnosis and its possible treatments. But the anesthesia affected my judgment. Thankfully, I was thinking more clearly after the news about my insurance.
My research led me to an obscure web site run by Howard H. Wayne a renegade cardiologist in San Diego. Dr. Wayne is a rare commodity in medicine: he cares more about his patients than the bottom line. A master of customer service, he personally oversees every aspect of his patients’ care.
Dr. Wayne said that bypass surgery is unnecessary in 98 percent of patients. But the $40,000 price tag for the procedure, versus the cost of simple medications, makes surgery attractive to the doctors who perform it.
Unfortunately, statistics show that 53 percent of patients who undergo the surgery or angioplasty are likely to die or have a heart attack within five years. Those treated with medication have only a 5 percent chance of this outcome. In addition, those who are 56 years young, as I am, likely face a repeat bypass operation within 20 years.
I had been told by the surgeon that while my arteries were clogged, my heart was strong. This makes little sense because a heart can be strong only when it receives sufficient oxygen, which theoretically would not be possible with 90-percent and 100-percent blockages. What the surgeon and cardiologist didn’t tell me was that the body creates its own bypass system, making surgery not only unnecessary but detrimental.
After visiting Dr. Wayne, I learned that my chest tightness, as is almost always the case, was caused by high blood pressure. Interestingly, my blood pressure was normal – at rest. That is how most physicians record it. But Dr. Wayne likes to see how blood pressure performs under stress. My resting blood pressure was 120/70, perfectly normal. But Dr. Wayne performed a non-invasive test, asking me to squeeze a handgrip measuring instrument for one minute. The result: 140/110. It could have been as high as 200/150, he said, if my primary care physician had not already started me on beta blockers.
Since early June, I have been on a regimen of several medications that have lowered my blood pressure to 90/50. This may sound far too low, but Dr. Wayne said plaque in the arteries is encouraged by blood coursing through too quickly, causing injury. The lower the blood pressure, he says, the less chance for such injury.
And have I mentioned, that I haven’t had the chest tightness or shortness of breath since starting his regimen? According to Dr. Wayne, I am likely to live a long, full life. I am very grateful to the surgeon who was not in network with my insurance company and Dr. Wayne for that.
Like Clinton, I began to experience chest tightness earlier this year. Ironically, it happened whenever I did the one thing we’re always told we don’t do enough of: exercise. I’d walk only a few blocks, and I’d feel a non-painful chest tightness and shortness of breath. It went away when I was at rest.
In April, my primary care physician performed an EKG that appeared normal. Even so, she felt that I should consult a cardiologist and seek further tests. The cardiologist at the state-of-the-art, multi-million dollar Indiana Heart Hospital ordered a stress test and imaging study of my heart, the results of which were deemed “abnormal.”
The cardiologist scheduled me for an angiogram, an invasive procedure in which a catheter with a camera on the end is inserted in the leg and threaded into the heart to get a closer look. I was warned that I likely had blockages in one or more coronary arteries that would require the placement of stents.
The doctor’s reaction when I requested the procedure to be postponed until May because of a planned vacation led me to believe that my situation was not life-threatening.
At 5:30 a.m. on May 10, I arrived at the four-star hotel they call the Indiana Heart Hospital for the outpatient procedure. A guest relations representative escorted me through the double doors to a small room in Suite C.
As I emerged from my twilight sleep, I was double-teamed by my heart specialist and a cardiothoracic surgeon he had paged for an emergency consult. The specialist told me that I had massive blockages to each of my three coronary arteries and surrounding vessels that supply oxygen to my heart. He said so many blockages were involved that stents would not be effective. I would need a quintuple bypass.
The surgeon, summoning up his most understanding bedside manner, shared that he understood how I felt because he had undergone surgery recently himself. It was Monday, and he anticipated doing the surgery on Wednesday or Thursday. The surgeon explained that I would need pre-operative instruction, which would be best for me to do while still in the hospital.
On Wednesday night, I prepared for Thursday morning surgery just as the physical therapist and nurse had instructed. But that same nurse called and said that the surgeon was not in network with my insurance. The procedure would be postponed until a network surgeon could be found.
A retired Army nurse, I normally would be the first to conduct in-depth research into any diagnosis and its possible treatments. But the anesthesia affected my judgment. Thankfully, I was thinking more clearly after the news about my insurance.
My research led me to an obscure web site run by Howard H. Wayne a renegade cardiologist in San Diego. Dr. Wayne is a rare commodity in medicine: he cares more about his patients than the bottom line. A master of customer service, he personally oversees every aspect of his patients’ care.
Dr. Wayne said that bypass surgery is unnecessary in 98 percent of patients. But the $40,000 price tag for the procedure, versus the cost of simple medications, makes surgery attractive to the doctors who perform it.
Unfortunately, statistics show that 53 percent of patients who undergo the surgery or angioplasty are likely to die or have a heart attack within five years. Those treated with medication have only a 5 percent chance of this outcome. In addition, those who are 56 years young, as I am, likely face a repeat bypass operation within 20 years.
I had been told by the surgeon that while my arteries were clogged, my heart was strong. This makes little sense because a heart can be strong only when it receives sufficient oxygen, which theoretically would not be possible with 90-percent and 100-percent blockages. What the surgeon and cardiologist didn’t tell me was that the body creates its own bypass system, making surgery not only unnecessary but detrimental.
After visiting Dr. Wayne, I learned that my chest tightness, as is almost always the case, was caused by high blood pressure. Interestingly, my blood pressure was normal – at rest. That is how most physicians record it. But Dr. Wayne likes to see how blood pressure performs under stress. My resting blood pressure was 120/70, perfectly normal. But Dr. Wayne performed a non-invasive test, asking me to squeeze a handgrip measuring instrument for one minute. The result: 140/110. It could have been as high as 200/150, he said, if my primary care physician had not already started me on beta blockers.
Since early June, I have been on a regimen of several medications that have lowered my blood pressure to 90/50. This may sound far too low, but Dr. Wayne said plaque in the arteries is encouraged by blood coursing through too quickly, causing injury. The lower the blood pressure, he says, the less chance for such injury.
And have I mentioned, that I haven’t had the chest tightness or shortness of breath since starting his regimen? According to Dr. Wayne, I am likely to live a long, full life. I am very grateful to the surgeon who was not in network with my insurance company and Dr. Wayne for that.
WordWorks2001 Uncensored
I was posting on a message board at www.healthboards.com for several months and it was not an experience that was open to the free and unfettered exchange of ideas. So, I decided to start my own board. I may not get as many people noticing my writings as I did at HealthBoards, but I will be able to say my mind without fear of being banned.
And, anyone else who wishes to reply may do so, without far of censorship. But your words and ideas may be challenged. If that doesn't bother you, WRITE ON!
And, anyone else who wishes to reply may do so, without far of censorship. But your words and ideas may be challenged. If that doesn't bother you, WRITE ON!
Monday, September 06, 2004
Blood Pressure Report
I am doing well. The lightheadedness continues, some
days are more frequent than others. If I sit for a
while before rising and go slowly, I find the symptoms
subside quicker. I have not come close to passing
out, so its not very troubling. My BPs for August 15
through September 6, 2004 follow:
DATE TIME BP PULSE
08/15 1145 88/46 64
08/15 2200 98/56 70
08/16 0715 90/52 80
08/16 1515 102/58 76
08/16 2045 96/52 76
08/17 0700 104/62 62
08/17 1200 78/46 66
08/17 1630 80/44 60
08/18 1115 100/60 60
08/18 1445 112/60 60
08/18 1930 108/60 64
08/18 2315 90/52 68
08/19 0745 94/52 68
08/19 1400 104/56 78
08/19 1945 100/56 66
08/19 2245 88/50 66
08/20 1815 100/56 58
08/20 2130 96/52 62
08/21 1915 90/48 72
08/21 1945 98/54 64
08/21 2045 88/48 60
08/21 2145 92/48 60
08/22 1000 112/60 72
08/22 1930 92/52 60
08/22 2100 104/56 60
08/23 0830 106/48 66
08/23 1700 102/56 64
08/23 2200 92/52 54
08/24 0800 96/58 78
08/24 2030 96/54 88
08/24 2130 96/52 80
08/25 0800 106/58 64
08/25 2100 108/62 66
08/25 2215 104/58 64
08/26 0730 100/56 64
08/26 0930 96/52 66
08/26 2045 106/56 66
08/27 0830 108/58 62
08/27 1845 106/58 74
08/27 2030 104/58 66
08/28 1045 96/52 56
08/28 1345 88/48 64
08/28 2230 104/58 56
08/29 0945 88/52 66
08/29 1330 86/50 56
08/29 2130 86/46 56
08/29 2330 76/42 60
08/30 0800 86/50 60
08/30 1530 88/48 82
08/30 2245 96/58 58
08/31 1330 94/48 70
08/31 1900 104/56 70
08/31 2200 108/56 60
09/01 2000 96/52 66
09/01 2100 104/48 56
09/01 2230 86/48 58
09/02 2045 106/60 58
09/03 2000 100/56 64
09/03 2215 88/48 60
09/04 2200 88/48 66
09/04 2245 86/46 58
09/05 1330 84/46 64
09/05 1830 96/48 70
09/05 2345 82/48 60
09/06 1045 92/44 62
09/06 1915 106/58 82
09/06 2145 106/56 54
days are more frequent than others. If I sit for a
while before rising and go slowly, I find the symptoms
subside quicker. I have not come close to passing
out, so its not very troubling. My BPs for August 15
through September 6, 2004 follow:
DATE TIME BP PULSE
08/15 1145 88/46 64
08/15 2200 98/56 70
08/16 0715 90/52 80
08/16 1515 102/58 76
08/16 2045 96/52 76
08/17 0700 104/62 62
08/17 1200 78/46 66
08/17 1630 80/44 60
08/18 1115 100/60 60
08/18 1445 112/60 60
08/18 1930 108/60 64
08/18 2315 90/52 68
08/19 0745 94/52 68
08/19 1400 104/56 78
08/19 1945 100/56 66
08/19 2245 88/50 66
08/20 1815 100/56 58
08/20 2130 96/52 62
08/21 1915 90/48 72
08/21 1945 98/54 64
08/21 2045 88/48 60
08/21 2145 92/48 60
08/22 1000 112/60 72
08/22 1930 92/52 60
08/22 2100 104/56 60
08/23 0830 106/48 66
08/23 1700 102/56 64
08/23 2200 92/52 54
08/24 0800 96/58 78
08/24 2030 96/54 88
08/24 2130 96/52 80
08/25 0800 106/58 64
08/25 2100 108/62 66
08/25 2215 104/58 64
08/26 0730 100/56 64
08/26 0930 96/52 66
08/26 2045 106/56 66
08/27 0830 108/58 62
08/27 1845 106/58 74
08/27 2030 104/58 66
08/28 1045 96/52 56
08/28 1345 88/48 64
08/28 2230 104/58 56
08/29 0945 88/52 66
08/29 1330 86/50 56
08/29 2130 86/46 56
08/29 2330 76/42 60
08/30 0800 86/50 60
08/30 1530 88/48 82
08/30 2245 96/58 58
08/31 1330 94/48 70
08/31 1900 104/56 70
08/31 2200 108/56 60
09/01 2000 96/52 66
09/01 2100 104/48 56
09/01 2230 86/48 58
09/02 2045 106/60 58
09/03 2000 100/56 64
09/03 2215 88/48 60
09/04 2200 88/48 66
09/04 2245 86/46 58
09/05 1330 84/46 64
09/05 1830 96/48 70
09/05 2345 82/48 60
09/06 1045 92/44 62
09/06 1915 106/58 82
09/06 2145 106/56 54
Sunday, August 15, 2004
Blood Pressure Report
Here is my BP Report for 07/13/04 thru 08/14/04.
DATE TIME BP PULSE
07/13 1400 106/70 66
07/17 1830 90/56
76
07/18 1300 94/62
64
07/19 0900 96/64
88
07/19 1900 88/56
82
07/24 1200 90/56
88
07/28 2115 108/60 74
07/28 2330 110/62 72
07/29 1400 86/50
70
07/29 2015 102/54 68
07/30 2045 106/64 56
07/30 2045 110/64 58
07/31 1800 96/54
74
07/31 2100 106/60 64
08/01 1615 106/60 60
08/01 2200 102/62 68
08/02 0745 100/58 56
08/02 1300 94/52
64
08/02 1945 106/50 74
08/03 0715 106/52 58
08/03 1900 88/48
74
08/03 2100 102/68 74
08/04 0715 102/56 58
08/04 0945 80/46
70
08/04 1330 102/58 82
08/04 1545 88/50 66
08/05 0800 100/56 56
08/05 1630 102/60 84
08/07 0000 100/58 54
08/07 0945 102/54 60
08/07 0000 96/54 62
08/08 1830 96/52 50
08/10 1935 86/48 88
08/11 0715 108/58 60
08/12 1900 116/66 56
08/12 2315 96/56 66
08/13 2045 96/54 82
08/13 2315 100/56 76
08/14 0945 88/56 66
08/14 2100 106/58 62
I began my Isordil this morning, taking 1/2 tablet. I
will take one tablet in 6 hours. So my daily dosage
will be 1/2 tab in the early morning and 1 tab 6 hours
later. Correct?
How am I doing so far. I still get lightheaded
occassionally, but those incidents are decreasing in
number and intensity. I did experience some very
minor chest tightness while on a rather long walk on
Friday. It stopped by itself without resting or
taking any NTG.
Jeff
DATE TIME BP PULSE
07/13 1400 106/70 66
07/17 1830 90/56
76
07/18 1300 94/62
64
07/19 0900 96/64
88
07/19 1900 88/56
82
07/24 1200 90/56
88
07/28 2115 108/60 74
07/28 2330 110/62 72
07/29 1400 86/50
70
07/29 2015 102/54 68
07/30 2045 106/64 56
07/30 2045 110/64 58
07/31 1800 96/54
74
07/31 2100 106/60 64
08/01 1615 106/60 60
08/01 2200 102/62 68
08/02 0745 100/58 56
08/02 1300 94/52
64
08/02 1945 106/50 74
08/03 0715 106/52 58
08/03 1900 88/48
74
08/03 2100 102/68 74
08/04 0715 102/56 58
08/04 0945 80/46
70
08/04 1330 102/58 82
08/04 1545 88/50 66
08/05 0800 100/56 56
08/05 1630 102/60 84
08/07 0000 100/58 54
08/07 0945 102/54 60
08/07 0000 96/54 62
08/08 1830 96/52 50
08/10 1935 86/48 88
08/11 0715 108/58 60
08/12 1900 116/66 56
08/12 2315 96/56 66
08/13 2045 96/54 82
08/13 2315 100/56 76
08/14 0945 88/56 66
08/14 2100 106/58 62
I began my Isordil this morning, taking 1/2 tablet. I
will take one tablet in 6 hours. So my daily dosage
will be 1/2 tab in the early morning and 1 tab 6 hours
later. Correct?
How am I doing so far. I still get lightheaded
occassionally, but those incidents are decreasing in
number and intensity. I did experience some very
minor chest tightness while on a rather long walk on
Friday. It stopped by itself without resting or
taking any NTG.
Jeff
Tuesday, July 13, 2004
Blood Pressure Report & Questions
I am feeling well. There is some occasional "aching"
feelings on both sides of my upper chest, which I
attribute to muscle cramping or chest wall type pain.
Twice since I last communicated with you, I
experienced some shortness of breath. These
occurrences were while walking up hill in 90 degree
plus heat. I cannot say I have had any chest
tightness, a la the symptoms I had before beginning
the medical program you have me on.
The most frequent symptom I have, occurring once or
twice a day for as long as a couple of hours, is
lightheadedness. Sometimes it is quite noticeable,
but I have not felt like "passing out." I also have
heartburn on several days a week, which I attribute to
gastric reflux and is fairly well relieved with
Pepsid.
I began taking Fosinopril 10 mg at bedtime on Sunday
evening. I noticed this morning that I actually was
supposed to begin it on July 18, so I mistakenly
jumped the gun by one week.
Here are my vital signs since my last report:
Date Time BP P
06/23 7:45 am 110/58 68
06/23 4:00 pm 110/80 80
06/23 8:25 pm 110/64 80
06/24 7:00 pm 100/74 64
06/24 9:00 pm 90/56 68
06/25 8:45 am 90/60 74
06/25 9:25 pm 100/58 76
06/26 11:00am 96/60 58
06/26 6:00 pm 110/76 58
06/27 10:30am 92/58 70
06/27 noon 90/60 76
06/27 6:00 pm 96/60 76
06/27 10:00pm 90/64 62
06/28 7:00 am 100/70 70
06/28 8:45 pm 120/86 * 92 *
06/29 9:30 pm 90/58 76
07/01 10:38am 96/62 76
07/01 11:00pm 110/66 74
07/02 8:00 am 100/70 68
07/03 8:00 am 108/80 66
07/03 5:40 pm 90/60 84
(07/04 - Moduretic increased to 2 tabs q am)
07/04 9:20 am 100/60 60
07/04 8:00 pm 94/68 70
07/05 8:30 am 86/58 66
07/06 8:30 am 110/64 68
07/07 6:00 pm 100/62 66
07/08 11:30am 90/62 68
07/08 7:30 am 86/60 86
07/09 8:20 am 120/56 76
07/09 6:40 pm 100/60 84
07/09 10:40pm 100/56 68
07/10 4:00 pm 130/80 76
07/11 5:45 pm 92/76 74
07/11 8:20 pm 100/72 88
07/11 10:30pm 90/72 66
07/12 4:30 pm 100/58 60
07/13 8:40 am 90/62 64
Now for the questions:
My neurologist wants me to take Lipitor 10 qd because
of plaque in my carotid arteries he says can lead to
stroke. I told him I really don't want to take it and
he cited patients he has had on statins for 10 to 15
years who have actually demonstrated a lessening of
athersclerosis in their carotids over the years. I
told him I would run it by you.
Would Lipitor be contraindicated with any of the
medications I am now on?
These symptoms of lightheadedness: They are somewhat
disconcerting, particularly when I am at a social
event. They do not seem to be related to activity or
food or alcohol ingestion.
Will these symptoms subside or get worse as I increase
the dosages and amounts of medication I am taking?
Do you have any suggestions for treating the
lightheadedness?
Given the fact I started the Fosinopril a week early
by mistake, should I adjust the dates I am to increase
it or go back to the schedule as outlined in the
medical program you provided me on June 2?
I guess that's all from this end. Hope you had a
great Independence Day weekend. Rebecca and I did.
We went to New York City and saw a Broadway show and
then went on to Connecticut to visit my mother. This
week we are in Nashville for a conference.
Jeff
feelings on both sides of my upper chest, which I
attribute to muscle cramping or chest wall type pain.
Twice since I last communicated with you, I
experienced some shortness of breath. These
occurrences were while walking up hill in 90 degree
plus heat. I cannot say I have had any chest
tightness, a la the symptoms I had before beginning
the medical program you have me on.
The most frequent symptom I have, occurring once or
twice a day for as long as a couple of hours, is
lightheadedness. Sometimes it is quite noticeable,
but I have not felt like "passing out." I also have
heartburn on several days a week, which I attribute to
gastric reflux and is fairly well relieved with
Pepsid.
I began taking Fosinopril 10 mg at bedtime on Sunday
evening. I noticed this morning that I actually was
supposed to begin it on July 18, so I mistakenly
jumped the gun by one week.
Here are my vital signs since my last report:
Date Time BP P
06/23 7:45 am 110/58 68
06/23 4:00 pm 110/80 80
06/23 8:25 pm 110/64 80
06/24 7:00 pm 100/74 64
06/24 9:00 pm 90/56 68
06/25 8:45 am 90/60 74
06/25 9:25 pm 100/58 76
06/26 11:00am 96/60 58
06/26 6:00 pm 110/76 58
06/27 10:30am 92/58 70
06/27 noon 90/60 76
06/27 6:00 pm 96/60 76
06/27 10:00pm 90/64 62
06/28 7:00 am 100/70 70
06/28 8:45 pm 120/86 * 92 *
06/29 9:30 pm 90/58 76
07/01 10:38am 96/62 76
07/01 11:00pm 110/66 74
07/02 8:00 am 100/70 68
07/03 8:00 am 108/80 66
07/03 5:40 pm 90/60 84
(07/04 - Moduretic increased to 2 tabs q am)
07/04 9:20 am 100/60 60
07/04 8:00 pm 94/68 70
07/05 8:30 am 86/58 66
07/06 8:30 am 110/64 68
07/07 6:00 pm 100/62 66
07/08 11:30am 90/62 68
07/08 7:30 am 86/60 86
07/09 8:20 am 120/56 76
07/09 6:40 pm 100/60 84
07/09 10:40pm 100/56 68
07/10 4:00 pm 130/80 76
07/11 5:45 pm 92/76 74
07/11 8:20 pm 100/72 88
07/11 10:30pm 90/72 66
07/12 4:30 pm 100/58 60
07/13 8:40 am 90/62 64
Now for the questions:
My neurologist wants me to take Lipitor 10 qd because
of plaque in my carotid arteries he says can lead to
stroke. I told him I really don't want to take it and
he cited patients he has had on statins for 10 to 15
years who have actually demonstrated a lessening of
athersclerosis in their carotids over the years. I
told him I would run it by you.
Would Lipitor be contraindicated with any of the
medications I am now on?
These symptoms of lightheadedness: They are somewhat
disconcerting, particularly when I am at a social
event. They do not seem to be related to activity or
food or alcohol ingestion.
Will these symptoms subside or get worse as I increase
the dosages and amounts of medication I am taking?
Do you have any suggestions for treating the
lightheadedness?
Given the fact I started the Fosinopril a week early
by mistake, should I adjust the dates I am to increase
it or go back to the schedule as outlined in the
medical program you provided me on June 2?
I guess that's all from this end. Hope you had a
great Independence Day weekend. Rebecca and I did.
We went to New York City and saw a Broadway show and
then went on to Connecticut to visit my mother. This
week we are in Nashville for a conference.
Jeff
Tuesday, June 22, 2004
Blood Pressure Report to Dr. Wayne
I took my evening dose of Metoprolol 75mg at about 7
pm. I began feeling somewhat lightheaded while doing
some cleanup work at about 7:30 pm. I have been
resting since 8:30 or so and the light headedness
continues at 10:30 pm. My BP is 88/50 and my pulse is
70. I went from 50mg to 75mg on Sunday. Should I
continue this dosage?
Here are my readings since the last e-mail I sent you:
Date/Time BP Pulse
Activity
06-15/7:45AM 110/78 76
resting
06-15/1:45PM 126/76 76
resting
06-15/6:30PM 102/64 80
resting
06-16/7:45AM 106/78 72
awoke
06-16/7:45PM 114/90 76 ate
supper
06-17/5:30PM 116/68 84
resting
06-18/Noon 116/66 76
ate lunch
06-19/9:00PM 100/70 84
resting after concert
06-20/7:45AM 116/64 64
awoke
06-20/11:30AM 100/66 68
resting
06-20/6:45PM 100/64 84 ate
dinner
06-20/10:30PM 112/78 80
watching TV
06-21/1:30PM 110/74 76
resting
06-21/9:30PM 106/58 68
resting
06-22/5:00PM 120/70 68
resting
06-22/10:30PM 88/50 70
resting
I only had one incident of chest tightness since
starting the medical program. That was last evening
when I was doing some rather strenuous work. It was
relieved by a few minutes of rest and did not return.
Jeff
pm. I began feeling somewhat lightheaded while doing
some cleanup work at about 7:30 pm. I have been
resting since 8:30 or so and the light headedness
continues at 10:30 pm. My BP is 88/50 and my pulse is
70. I went from 50mg to 75mg on Sunday. Should I
continue this dosage?
Here are my readings since the last e-mail I sent you:
Date/Time BP Pulse
Activity
06-15/7:45AM 110/78 76
resting
06-15/1:45PM 126/76 76
resting
06-15/6:30PM 102/64 80
resting
06-16/7:45AM 106/78 72
awoke
06-16/7:45PM 114/90 76 ate
supper
06-17/5:30PM 116/68 84
resting
06-18/Noon 116/66 76
ate lunch
06-19/9:00PM 100/70 84
resting after concert
06-20/7:45AM 116/64 64
awoke
06-20/11:30AM 100/66 68
resting
06-20/6:45PM 100/64 84 ate
dinner
06-20/10:30PM 112/78 80
watching TV
06-21/1:30PM 110/74 76
resting
06-21/9:30PM 106/58 68
resting
06-22/5:00PM 120/70 68
resting
06-22/10:30PM 88/50 70
resting
I only had one incident of chest tightness since
starting the medical program. That was last evening
when I was doing some rather strenuous work. It was
relieved by a few minutes of rest and did not return.
Jeff
Subscribe to:
Comments (Atom)