A noninvasive procedure for treating angina has proven nearly as effective as angioplasty, said a cardiologist who has been using Enhanced External Counterpulsation for his patients for the past several years.
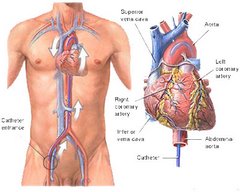
A noninvasive procedure for treating angina has proven nearly as effective as angioplasty, said a cardiologist who has been using Enhanced External Counterpulsation for his patients for the past several years. Dr. James P. O’Neil, a cardiologist with the Cardiology Group, which administers the procedure at its Mount Laurel office, said coronary angioplasty, a medical procedure which involves inserting a balloon catheter to open a blockage in an artery, and the EECP offer patients “about the same success rate.”
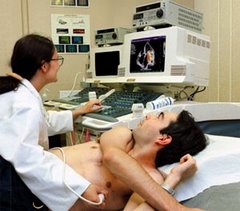
During EECP, cuffs similar to blood pressure cuffs that have been wrapped around patients’ legs are inflated and deflated, forcing blood to flow through arteries. “The body reacts by improving collateral blood flow” with small capillaries expanding to compensate for the blocked artery, said O’Neil.
He said the aim of both procedures is to “improve exercise tolerance and fatigue,” common problems for heart patients.
Angina is a symptom related to coronary heart disease. Blockages in coronary arteries created by the buildup of plaque on the inner walls of the vessels limit the supply of oxygen-rich blood to the heart and cause the chest pain or discomfort known as angina and shortness of breath.
O’Neil said medications are usually the first step in an attempt to ease the discomfort, but if they do not work, then cardiac bypass surgery, angioplasty or EECP treatments should be considered.
He said EECP relieves symptoms in 75 percent of cases, “a little bit less than angioplasty,” which eases symptoms in 80 percent of cases. Cardiac bypass surgery improves symptoms 90 percent of the time, said O’Neil.
O’Neil said The Cardiology Group, which has five offices in Burlington County, has done nearly 300 of the lower risk EECP procedures since it began offering EECP six years ago. The procedure is administered the same now as when it was introduced, in one-hour sessions five days a week for seven weeks.
The time commitment is the only disadvantage of using EECP, said O’Neil, who cited several advantages of using it instead of angioplasty to relieve angina.
“Angioplasty is three times the cost as the EECP, the risk is higher, there is no survival advantage of angioplasty over EECP,” said O’Neil.
O’Neil said a report issued during a recent American College of Cardiology conference supported the view that the two procedures offer similar success.
“We used to think that people lived longer (by having angioplasty),” he said. “Angioplasty is really stretching the vessel and really tearing the vessel. During angioplasty, that vessel is damaged and as it heals, it can cause a scar.”
The resulting scar can create a new blockage, although a drug-eluding stent sometimes is used to hinder the scar buildup, he said.
“One out of 10 patients tend to block up again with that artery,” he said. “With EECP, we’re not damaging an artery and causing scar tissue to build up.
“The big thing that has been found with EECP, a patient is not going to die any more often than those who have angioplasty. There’s a big misconception that if we do angioplasty it’s going to make them live longer.”
An exception, he said, is that when performed during a heart attack, angioplasty can serve as a lifesaving procedure.
O’Neil compared the effectiveness of the three procedures used in relieving angina. He said cardiac bypass surgery improves symptoms in 90 percent of cases, angioplasty in 80 percent and EECP in 75 percent.
The cardiologist said some insurance carriers, including Medicare, only recommend EECP as a remedy for patients who are not considered candidates for cardiac bypass surgery or angioplasty.
“I and many physicians don’t agree. We think EECP should be offered along with bypass and angioplasty,” O’Neil said. “One of the reasons patients don’t want bypass is they are afraid.”
He said insurance regulations sometimes deter patients from taking advantage of EECP.
“One of the biggest obstacles is how the insurance companies can make it difficult. They can and do make it difficult for patients to go through this,” said O’Neil, noting that out-of-pocket charges such as per-visit co-pays can deter patients from having the treatments.
“They might not have as big an out-of-pocket expense if they take the riskier, higher priced procedure,” he said.
O’Neil said EECP costs $6,000 to $7,000 whereas the angioplasty costs $20,000 to $30,000.
Patients who have had EECP say they are happy with the results.
That includes the Cardiology Group’s first EECP patient.
At 83, Nick Russo still mans a tractor to cultivate the pumpkin patch at the family farm in Chesterfield. In March 2001, he was the first patient to undergo EECP at the Cardiology Group.
Although Russo stashes a bottle of nitroglycerin pills in his pocket — just in case — the Westampton man said he hasn’t needed any of the medication since 2003, when a second round of EECP treatments seemed to ease the lingering angina.
Russo, who was diagnosed with a heart problem 10 years ago, underwent an open heart procedure at Deborah Heart and Lung Center in Browns Mills, Pemberton Township, in 1999. He took nitroglycerin to ease angina, eventually deciding to have the EECP.
Russo said his initial EECP treatments were “a little frightening at first. You get a shock.”
After having the EECP in 2001, Russo said, “I would still get out of breath. Once in awhile I would have to take a nitro pill.”
He said he noticed the angina “when I would do anything that was exertion” — lifting bags of fertilizer, loading crates of corn — and his cardiologist suggested a second set of treatments.
Marlene Donnelly of the Cardiology Group said EECP can be repeated “as long as it’s medically indicated.” She said one patient has had three sessions of EECP.
Angioplasty also may be repeated, Donnelly said.
After having a second angioplasty last July (the first was in May 2006), Edward Stickel of Delanco “felt better for a while, and then I started to experience unstable angina. For about 11 consecutive days in September and October I had angina in my left shoulder,” he said.
Stickel, 68, said cardiologist Samuel Ventrella thought EECP would help. He started the treatments on Nov. 6, and after about 12 sessions “started to feel much better.” By Dec. 6, “I stopped having the angina,” said Stickel, who retired from teaching at Palmyra High School, where he also coached freshman football for 18 years. He enrolled in the Cardiology Group’s rehab program, and exercises at the Mount Laurel center twice a week.
The former educator also said he is still able to go waterfowl hunting and fly fishing.
Stickel said he is covered by Medicare and by a Blue Cross/Blue Shield plan and was not troubled by the cost of the EECP treatments.
“I was charged a $5 co-pay, which I found to be not a real problem,” he said.
Jane Tabone-Yerkes of Pemberton Township, who is covered by a Civil Service insurance plan, said she had no co-pay for her EECP treatments, which she completed on Feb. 5.
Diagnosed with a heart problem 17 years ago, Tabone-Yerkes, 76, said, “I feel wonderful. I can go up the steps, I go up and down and I have no problem.”
Tabone-Yerkes, who had a stent inserted following a heart attack in 2005, said she asked her cardiologist for the EECP after reading about the procedure in a magazine. She said a second bypass surgery was not recommended.
During the procedure, “You are plummeted,” said Tabone-Yerkes, describing the sensation.
“It’s like a boxer socking you in every blood vessel of your body, but it was not hard to take,” she said.
Tabone-Yerkes said her angina, which she felt “down one arm,” “disappeared completely after 15 sessions.
“I felt like I did when I had the bypass 17 years ago,” she said.
A nitroglycerin tablet is part of her daily pill regimen, which also includes medications to control diabetes, high cholesterol and high blood pressure. Tabone-Yerkes, who retired from her job as an accounting technician at McGuire Air Force Base, said a low-fat diet and swimming five laps each morning in her pool helps her stay fit, and she recently joined a fitness center that caters to cardiac patients.
She said EECP was a good choice.
“They used to say it’s the last resort, but I don’t think that’s true,” said Tabone-Yerkes.
(from the Burlington County Times)